Servicios Personalizados
Revista
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309versión impresa ISSN 1681-150X
SA orthop. j. vol.22 no.1 Centurion 2023
https://doi.org/10.17159/2309-8309/2023/v22n1a7
HAND
A subungual glomus tumour of the finger with five reappearances: a rare case report
Collen S NkosiI, *; Tatolo I SefeaneII
IChris Hani Baragwanath Academic Hospital, Department of Orthopaedic Surgery, University of the Witwatersrand, Johannesburg, South Africa
IIHands Unit, Chris Hani Baragwanath Academic Hospital, Department of Orthopaedic Surgery, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND: A subungual glomus tumour is a rare benign neoplasm that develops in the distal portion of the finger from the glomus body. Hand surgeons are most significant in the diagnosis of this tumour
CASE REPORT: We present an atypical case of a patient who experienced multiple recurrences of a subungual glomus tumour of the finger over a period of 26 years. A transungual approach was used to remove the nail during the surgical excision. Postoperatively, the patient was symptom-free
DISCUSSION: The glomus body is the neuromyoarterial histological structure located in the stratum reticularis of the dermis of the skin and the subungual regions. Recurrences can be classified as early, delayed and ancient. Early recurrences may result from incomplete excision or a second tumour that develops within a year of the initial excision. A year following excision, delayed recurrences are thought to be caused by a new glomus tumour at the fingertip. A tumour that reappears more than three times after excision on the same fingertip in five years can be either a new or incomplete excised tumour, as in our case, and is considered an ancient recurrence. Surgical eye loupes should be use intraoperatively to improve complete tumour lesion excision
CONCLUSION: To the best of our knowledge, this is the first case of a finger with five recurrences post excision. In the event that excision-related pain is significant, recurrence should be considered. Delayed and ancient recurrences are thought to be caused by a new glomus tumour at the fingertip that one cannot prevent with surgery
Level of evidence: Level 5
Keywords: recurrence, glomus tumour, finger, surgery
Introduction
A subungual glomus tumour is a rare benign neoplasm that develops in the distal portion of the finger from the glomus body.1 They account for 1-6% of all soft tissue tumours in the upper limb, particularly the hand (50-75%).2 The aetiology of the tumour is unknown.2 Because of its rarity, there is usually a significant period between the beginning of symptoms and the diagnosis.1,3 Sefeane et al. reported up to 16 years delay in diagnosis in 2013.1 Clinically, subungual glomus tumours are characterised by a classic triad of cold intolerance, localised tenderness and paroxysmal pain.3,4 Recurrences are seen in 4-15% within one year of excision.5
We present an atypical case of a patient who experienced five recurrences of a subungual glomus tumour of the finger over a period of 26 years.
Case report
A 65-year-old female presented with a worsening pain in the right subungual middle finger for the past six months. The pain was excruciating and affected her activities of daily living. She had had four previous surgical excisions (years: 1996, 2004, 2013 and 2015) with positive histology results of glomus tumour from the same middle finger. The longest period she was symptom-free was six years after resection.
On clinical examination of the right middle finger, there was typical triad of a bluish discolouration, a positive Love's pin test and a positive Hildreth's test with a split nail plate (Figure 1). The range of motion of the distal interphalangeal joint was normal.

Standard radiography showed an indentation on the dorsal surface of the distal phalanx of the middle finger, most likely due to previous surgery. Laboratory findings were within normal ranges. The affected middle finger was scanned using magnetic resonance imaging (MRI) and it revealed a subungual high signal intensity on T2 weighted and an isointense signal on T1 weighted images (Figure 2). The soft tissue lesion measured 4.3 * 1.7 * 4.1 mm. Histopathological assessment of the soft tissue excised from the distal phalanx with haematoxylin and eosin (H & E) * 100 and * 400 stain revealed blood vessels associated with round cells in a myxoid stroma. The tumour was confirmed by an immunostain with S-100 (Figure 3).
Subungual leiomyoma, subungual exostosis and subungual neuroma can be differentiated as subungual glomus tumours based on their clinical presentation.
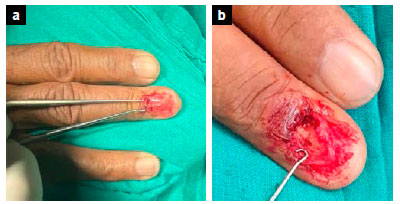
An excisional biopsy was performed under general anaesthesia, and a tourniquet was used to obtain a bloodless field. A transungual approach was used to remove the nail during the surgical excision. Using a McDonald's dissector, the nail plate was delicately raised from the nail bed and gently peeled out with an arterial forceps. Multiple small bluish soft tissue masses were identified on the subungual surface (Figure 4a). The tumour lesions were excised completely, and haemostasis was achieved by direct pressure (Figures 4b and 4c). The nail bed was closed with intermittent buried Monocryl sutures, and the patient's nail plate was used as a nailbed dressing sutured with Monocryl (Figure 4d). The lesions were sent for histopathological analysis, and the diagnosis of a subungual glomus tumour was confirmed.
The nailbed healed in 12 weeks (Figure 5); postoperative radiographs at 12 weeks showed a similar dimple to the preoperative radiographs (Figure 6); and the patient was symptom-free.


Discussion
Background
The glomus body is the neuromyoarterial histological structure located in the stratum reticularis of the dermis of the skin and the subungual regions. It comprises nerve fibres, modified smooth muscle cells termed glomus cells, afferent arterioles, collecting venules and arteriovenous anastomoses known as the Sucquet-Hoyer canal. It regulates the body's temperature and blood pressure through arteriovenous flow.1,2,4,6-8
Glomus tumour was originally described as 'painful subcutaneous tubercle' by Wood in 1812.9 In 1924, Mason et al. named glomus tumour following a histopathology analysis.10 They are commonly found on the distal parts of the fingers.2,11 After excision, there have been reports of a significant recurrence rate.5,6 It affects more middle-aged women than men.2,6 Recurrences can be classified as early, delayed and ancient.
Early recurrences may result from incomplete excision or a second tumour that develops within a year of the initial excision.6,12 A year following excision, delayed recurrences are thought to be caused by a new glomus tumour at the fingertip.6,12 A tumour that reappears more than three times after excision on the same fingertip in five years can be either a new or incomplete excised tumour as in our case, and the cases reported by Patel et al. and Dailiana et al. are considered an ancient recurrence.2,12 The skin-coloured tumours, as opposed to the traditional red, blue or purple glomus tumours, are challenging to distinguish during surgery, which raises the risk of recurrence.13,14
Clinical presentation
Clinically, glomus tumours are classified either solitary or multiple.5,11 Multiple tumours are asymptomatic and present in the young patient. In contrast, solitary subungual glomus tumours are characterised by a classic triad of cold intolerance, localised tenderness and paroxysmal pain.3,5 A nail plate deformity or split was previously reported and our case had a split nail plate.5,14
Despite a classical presentation and finger assessment, the tumour can be misdiagnosed for up to 15 years due to medical doctors' lack of exposure to the condition.13 Fawzi et al. reported an early diagnosis of the tumour by an experienced hand surgeon.15
The tumour is confirmed using various clinical tests. These include the Love's pin test, which has a 100% sensitivity and 78% accuracy, the Hildreth test, which has a 71.4% sensitivity, 91% specificity and 78% accuracy, and a cold sensitivity test, with 100 sensitivity, specificity and accuracy.1,5,6
Investigation
Plain radiographs can reveal a distal phalanx bone erosion or a cortical defect of the underlying bone.2,5,6 Our case had an indentation of the cortex. Ultrasonography is a valuable tool to use to confirm the site, size and shape of the glomus tumour, but it is highly operator dependent.2,5,6,14 MRI is the study of choice to establish the diagnosis; it helps with preoperative planning to assess the tumour size and location, which minimises the risk of incomplete excision.2,5 The classic features on MRI include a high signal core dot bordered by a zone of low signal intensity.2,15 The tumour lesion exhibits low signal intensity on T1 weighted, high signal intensity on T2 weighted, and enhancement on T1 weighted images following gadolinium administration.2,5,6,11,13
In this case, the tumour lesion was histologically confirmed as a glomus tumour. When compared to the earlier histology findings for this patient, there was no appreciable difference in the histology characteristics of the tumour that returned. Glomus cells present with nest-like epithelioid cells with eosinophilic cytoplasm and round nuclei following haematoxylin adenosine staining. Immunohistochemistry staining is used to excluded other tumour lesions from glomus tumour. It is positive for smooth muscle actin and vimentin, whereas cytokeratin and S-100 are immunonegative.7,11,15
Treatment
The literature reports varying rates of recurrence, but an excisional biopsy is regarded as the gold standard intervention option.15 In this case, the traditional transungual approach was done and it provided excellent exposure. It is advised that skin-coloured tumours be removed piece by piece, including the complete capsule, to prevent recurrence.6,15 Surgical eye loupes should be used intraoperatively to improve complete tumour lesion excision. Literature supports the use of intraoperative ultrasound or microscope to decrease risk of recurrence. A perioperative single or double tourniquet is advisable to keep a bloodless field during surgery.2,6
Recurrence
Recurrence was previously reported to be 4-15% within one year of excision, but current literature has provided data with a higher recurrence rate of 4-50%.6,10 Glomus tumours seldom turn malignant, and there are very few examples that have been documented in the literature.8,11,15
Conclusion
Recurrence of subungual glomus tumour after excision is uncommon, and fewer cases are known to have recurred after five years. In a woman who has historically had a tumour presenting with a triad of symptoms, recurrence of the tumour should be suspected, and an MRI must be performed to confirm it. The transungual approach provides excellent clinical outcomes for patients, but patients need to be informed of the possibility of nail deformity. To reduce the risk of missed reappearance, orthopaedic surgeons should not discharge patients with glomus tumours from regular follow-up.
Ethics statement
Ethics committee approval was obtained from the University of the Witwatersrand Human Research Ethics Clearance certificate (Wits): M220778. All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed written consent was obtained from all patients for being included in the study.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
CSN: conceptualisation, data collection, work design, manuscript preparation TIS: conceptualisation, manuscript approval and supervision of the study
ORCID
Nkosl CS https://orcid.org/0000-0002-6119-8466
Sefeane TI https://orcld.org/0000-0001-6579-7864
References
1. Sefeane T, Aden A, and Peters F. Subungual glomus tumours: Report on 11 cases. SA Orthop J. 2013;12(3):42-45. [ Links ]
2. Patel J, Vaish A, Vaishya R, Singhal S. Reappearance of a glomus tumour of the finger after nine years-A rare case report and literature review. Journal of Orthopaedic Reports. 2022 Mar 1;1(1):38-41. https://doi.org/10.1016/j.jorep.2022.03.014 [ Links ]
3. Singh D. Subungual glomus tumour: rare but real. Indian J Vasc Endovasc Surg. 2015;2(3):115-17. https://doi.org/10.4103/0972-0820.166932 [ Links ]
4. Gandhi J, Yang SS, Hurd J. The anatomic location of digital glomus tumour recurrences. J Hand Surg Am. 2010;35(6):986-89. https://doi.org/10.10164.jhsa.2010.02.019 [ Links ]
5. Jalan D, Elhence A, Rathore DS, Maley DK. A recurred subungual glomus tumour of the thumb. BMJ Case Rep. 2016;2016:bcr2015212963. https://doi.org/10.1136/bcr-2015-212963 [ Links ]
6. Morey VM, Garg B, Kotwal PP. Glomus tumours of the hand: review of literature. J Clin Orthop Trauma. 2016 Oct 1;7(4):286-91. https://doi.org/10.10164.jcot.2016.04.006 [ Links ]
7. Zanjani LO, Shafiee Nia B, Vosoughi F, et al. An unusual case of chest wall glomus tumor presenting with axillary pain: a case report and literature review. Eur J Med Res. 2021 Dec;26(1):1-6. https://doi.org/10.1186/s40001-021-00518-6 [ Links ]
8. Saaiq M. Presentation and management outcome of glomus tumors of the hand. Arch Bone Jt Surg. 2021May;9(3):312. https://doi.org/10.22038/abjs.2020.47878.2367 [ Links ]
9. Wood W. On painful subcutaneous tubercle. Edinburgh Med J Surg. 1812;8:283-91. [ Links ]
10. Barre JA, Masson PV. Anatomy - clinical study of certain painful sub-ungual tumors (tumors of neuromyo-arterial glomus of the extremities). Bull Soc Dermatol Syph. 1924;31:48-59. [ Links ]
11. Chou T, Pan SC, Shieh SJ, et al. Glomus tumor: twenty-year experience and literature review. Ann Plast Surg. 2016;76:S35-40. https://doi.org/10.1097/sap.0000000000000684 [ Links ]
12. Dailiana ZH, Drape JL, VIET D. A glomus tumour with four recurrences. J Hand Surg Eur Vol. 1999 Feb 1;24(1):131-32. [ Links ]
13. Tang CY, Tipoe T, Fung B. Where is the lesion? Glomus tumours of the hand. Arch Plast Surg. 2013 Sep;40(05):492-95. https://doi.org/10.5999/aps.2013.40.5.492 [ Links ]
14. Lin YC, Hsiao PF, Wu YH, Sun FJ, Scher RK. Recurrent digital glomus tumor: analysis of 75 cases. Dermatol Surg. 2010;36(9):1396-400. https://doi.org/10.1111/j.1524-4725.2010.01647.x [ Links ]
15. Fazwi R, Chandran PA, Ahmad TS. Glomus tumour: a retrospective review of 15 years experience in a single institution. Malays Orthop J. 2011;5(3):8. https://doi.org/10.5704/MOJ.1111.007 [ Links ]
Received: August 2022
Accepted: October 2022
Published: March 2023
* Corresponding author: drcsnkosi@gmail.com
Editor: Dr Duncan McGuire, University of Cape Town, Cape Town
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.