Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151Print version ISSN 0038-2361
S. Afr. j. surg. vol.57 n.2 Cape Town Jun. 2019
https://doi.org/10.17159/2078-5151/2019/v57n2a2950
CASE REPORT
The conundrum of a resolving cavernous sinus syndrome
LM Ford; MN Mpanza; JR Ouma
University of Witwatersrand
SUMMARY
A middle-aged lady who presented with headaches and sudden onset of left cavernous sinus syndrome was found to have a left persistent primitive trigeminal artery (PPTA) on scans. The syndrome uniquely resolved spontaneously after a few days. Vascular variations in the region of the cavernous sinus should be actively sought in cross-sectional imaging performed for cavernous sinus syndrome.
Case Presentation:
A thirty-four-year-old female presented in March 2018 for evaluation of collapse, against a background of a ten-year history of headaches, recently increasing in intensity and intractable to analgesics. The patient was HIV seronegative, hypertensive on a single agent and had poorly controlled asthma. Her headache was frontotemporal and retro-orbital worsening on coughing and was associated with vomiting and blackouts. She went on to develop diplopia and a left ptosis. The provisional diagnosis at this point was either at transient ischemic attack or a benign neoplastic process.
On presentation she was afebrile with a blood pressure of 150/105 mmHg a pulse rate 64 beats per minute and respiratory rate of 16 breaths per minute. She was fully conscious and cooperative. She had a left sided ptosis (Figure 1), decreased movement of the left eye in all directions, diplopia and decreased sensation to soft touch and pin prick over the left forehead and maxilla. Sensation over the mandible was distinctly spared. These signs were consistent with a fallout of the left cranial nerves, III (Oculomotor), IV (Trochlear), VI (Abducens), V1 (Ophthalmic branch of Trigeminal) and V2 (Maxillary branch of Trigeminal), all of which pointed to a lesion in the left cavernous sinus. Biochemical tests urea and creatinine, full blood count and cerebrospinal fluid chemistry were all normal. MRI revealed a PPTA (Figure 2).


MRA confirms this and suggested an absent PCommA (Figure 3).

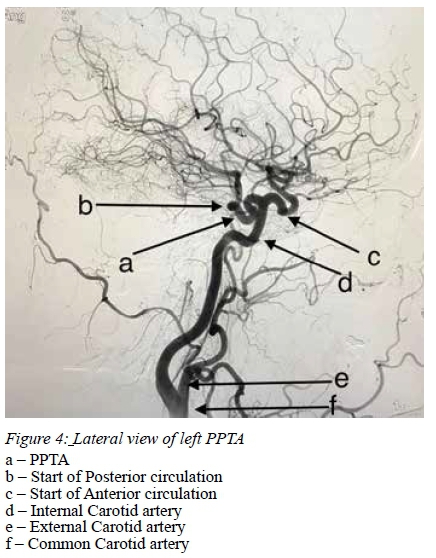
Formal Four-vessel Digital Subtraction Angiography (DSA) also confirmed a left PPTA (Figure 4).
The patient then had spontaneous resolution of cavernous sinus syndrome and all headaches.
Discussion:
Vasculogenesis, the process by which hemangioblasts differentiate into angioblasts, and angiogenesis, the formation of new vessels, are the two main stages of vascular embryology.
In the 4 mm foetal stage the hindbrain is supplied by two parallel neural arteries, which obtain their blood flow via the carotid-vertebrobasilar anastomoses from the trigeminal (TA), otic (OA), hypoglossal (HA) and pro-atlantal (ProA) arteries. The first and second brachial arches involute and the remnants are incorporated into the third arch and form the primitive internal carotid artery (ICA). Then the ICA gives rise to the cranial (primitive anterior cerebral artery (ACA)) and caudal PCommA divisions. The hindbrain is supplied in a rostro-caudal fashion by the longitudinal neural arterial group (TA, OA, HA). In the 5-6 mm foetal stage, the longitudinal neural arteries anastomose with the caudal end of the primitive ICA via the PCommA. The basilar artery (BA) forms during the 5-8 mm stage from the consolidation of the neural arteries.
The lifespan of the pre-segmental arteries regress TA, OA, and the HA is approximately a week, occurring after the posterior communicating artery (PComm) develops and connects with the distal BA.1
The causes of the persistence of normal embryonic arteries is not entirely clear. In some instances, it can be due to delay in the PComm development that would lead to an incomplete support to the distal BA and, with it, to a persistent need for these inferior anastomoses to maintain the flow. Other arguments state that the persistent embryonic arteries exist to make up for lack of appropriate flow from arteries normally present, i.e., hypoplastic PComm or a hypoplastic ICA.
Persistent primitive trigeminal artery (PPTA) is the most common of the 3 persistent carotid-vertebrobasilar anastomosis. Reported prevalence is 0.1-0.6%, average of 0.2%.1
It goes from the ICA to the BA, at the level of the cavernous sinus. It reaches the BA in 2 ways: in 50% of cases it penetrates the sella turcica, runs in its own groove and perforates the dura near the clivus to then join the BA between the anterior inferior cerebellar arteries (AICA) and the superior cerebellar arteries (SCA). In the other 50%, the TA leaves the cavernous sinus, courses with the trigeminal root, or runs between the sensory trigeminal root and the lateral side of the sella in a groove of the posterior petrosal process to join the BA between origins of the AICA and SCA.1
TA is an incidental finding in most reported cases, but can be associated with malformations such as aneurysms or anomalies in other blood vessels.
Saltzman et al. classified the angiographic appearance of PPTA by conventional angiography into 3 types according to their relationship with the neighbouring vessels. Type 1 is when TA joins the BA between the SCA and the AICA, the BA proximal to the junction is usually hypoplastic and the posterior communicating arteries (PCommA) are absent or poorly opacified. In Saltzman type 2 it also joins the BA between the SCA and AICA but the PCommA are present and supply the PCA. Saltzman type 3 is referred to the TA variant when it directly joins to a cerebellar artery.2 Weon et al. proposed that the PPTA could be reclassified into different types according to whether it supplies the contralateral PCA (type 3) or the ipsilateral PCA (type 4), type 1 and type 2 are the same as Saltzman's et al. type 1 and 2. Median and lateral types of PPTA are proposed by Salas et al. Previous reports presented these 2 types of PPTA according to the course of this vessel. The medial or sphenoidal type that is also associated with a pituitary adenoma and then the lateral or petrosal type that runs close to Meckel's cave.3 Knowledge of PPTA is important when considering surgery for other associated conditions such as transsphenoidal surgery for pituitary adenomas.

In most cases, the PPTA is an incidental finding, but its presence may be associated with malformations, aneurysms or anomalies in the other blood vessels. Patients may be asymptomatic or present with symptoms due to the flow of their posterior circulation or carotid microembolizations from the posterior circulation. In addition to these symptoms, PPTA can cause trigeminal neuralgia. Anatomical and angiographic studies have suggested that oculomotor nerve palsy, trigeminal neuralgia, and abducens nerve palsy might result from the lateral type of PPTA.3
PPTA has been associated previously with pituitary adenomas,4 as well as very rarely with skull base tumours.5 Cerebral angiography may assist with the decision to occlude the PPTA.5
A well-defined, rounded lesion similar to a vessel (observing the coronal section of the ICA in the cavernous sinus) should lead to suspicions of PPTA.4 Failure to recognize such anomalous vessels within the sella may lead to serious complications during transsphenoidal surgery. The DSA images suggest the patient has a Saltzman type 1 PPTA, where the PCommA is absent or poorly opacified.
As far as we are aware, there have been no previous reports of a Cavernous Sinus syndrome caused by a PPTA that has resolved spontaneously, as in this case.
Possible reasons for her presentation could have been a thrombosis, aneurysm, or fistula, all of which had been excluded with DSA. We speculate that a thrombosis of the cavernous sinus or ischaemia to the nerves could be the possible causes. In view of the marked ptosis we believe the former is most likely, although we have not seen a thrombosis resolving so quick.
Abbreviations
ACA - Anterior Cerebral artery AChA - Anterior Choroidal artery AICA - Anterior Inferior Cerebellar artery BA - Basilar artery HA - Hypoglossal artery ICA - Internal Carotid artery MCA - Middle Cerebral artery OA - Otic artery
PCommA - Posterior Communicating artery
PPTA - Persistent Primitive Trigeminal Artery
ProA - Proatlantal artery
SCA - Superior Cerebellar artery
TA - Trigeminal artery
VA - Vertebral artery
Declaration of interest: none
REFERENCES
1. Menshawi K, Mohr JP, Gutierrez J. A Functional Perspective on the Embryology and Anatomy of the Cerebral Blood Supply. J Stroke. 2015. [ Links ]
2. Pereira LP, Nepomuceno LAM, Coimbra PP, Neto SRDO, Natal MRC. Persistent trigeminal artery: Angio-tomography and angio-magnetic resonance finding. Arq Neuropsiquiatr. 2009. [ Links ]
3. Kim MJ, Kim MS. Persistent primitive trigeminal artery: analysis of anatomical characteristics and clinical significances. Surg Radiol Anat. 2014 [ Links ]
4. Machado MC, Kodaira S, Musolino NRC. Persistence of intrasellar trigeminal artery and simultaneous pituitary adenoma: description of two cases and their importance for the differential diagnosis of sellar lesions. Arq Bras Endocrinol Metabol. 2014 [ Links ]
5. Shen J, Tourje J, Chang EE, Mamelak AN, Wu AW. Persistent Trigeminal Artery in Endonasal Resection of Skull Base Tumors: A Systematic Review. J Neurol Surgery, Part B Skull Base. 2016. [ Links ]
 Correspondence:
Correspondence:
Dr Lauren M Ford
laurenford88@icloud.com













