Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.98 n.7 Pretoria Jul. 2008
ORIGINAL ARTICLES
Pre-operative clinical assessment for anaesthesia and the effect of HIV infection
P R PenfoldI; A C LundgrenII
IMB BCh, FCA (SA); Department of Anaesthesia, Chris Hani Baragwanath Hospital, Soweto, Johannesburg
IIMB ChB, FFA; Department of Anaesthesia, Chris Hani Baragwanath Hospital, Soweto, Johannesburg
ABSTRACT
BACKGROUND: HIV infection is common in South Africa, often remaining clinically latent and liable to be missed during clinical pre-operative assessment, despite the patient having a severe degree of immune compromise.
OBJECTIVES: The primary objective was to determine the pre-operative physical status of patients presenting for anaesthesia, and to compare this with subsequent HIV tests and the CD4 counts of the HIV-positive patients. The secondary objective was to determine the prevalence of HIV infection in this group and in selected subgroups.
METHOD: A sample of 350 adult patients presenting for anaesthesia at Chris Hani Baragwanath Hospital were interviewed pre-operatively, examined, and their American Society of Anesthesiologists physical status grading determined. In those who were confirmed HIV positive by blood sample, a CD4 count was checked. Further data were collected to determine trends in the characteristics of HIV-positive patients.
RESULTS: HIV-positive patients were more likely to be classified as ASA 1 or 2 than ASA 3 or 4 (odds ratio (OR) 2.1). HIV-positive patients with CD4 counts >200 cells/µl were more likely to be ASA 1 or 2 (OR 3.88). Of HIV-positive patients with CD4 counts <200 cells/µl, significantly more were classified as ASA 1 or 2 than ASA 3 or 4 (p<0.0001). Three patients with CD4 counts <50 cells/µl were classified as ASA 1 or 2. The overall prevalence of HIV infection was 29.4%. Females, patients presenting for obstetric surgery, and younger age groups had higher disease prevalence rates. Patients aged 30 - 39 years (43.0%) had the highest prevalence of HIV infection; the lowest was in patients aged 60 years or older (7.7%).
CONCLUSIONS: Routine clinical pre-operative assessment in patients from a population with a high HIV prevalence rate may result in asymptomatic, severe immune compromise being missed in a significant number of patients.
Sub-Saharan African countries have the highest prevalence of HIV infection in the world, at a rate of 7.2%, with South Africa ranking among the highest.1 Chris Hani Baragwanath Hospital (CHBH) is a 2 800-bed tertiary public hospital servicing a predominantly low-income population in Soweto, Johannesburg. It is well known for the volume of trauma surgery and other emergency surgery, including a busy obstetric unit (approximately 580 caesarean sections monthly, mostly as emergencies).
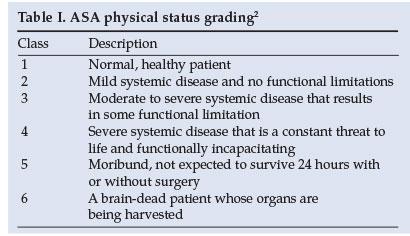
Patients are assessed pre-operatively to determine their physical fitness for the planned surgery and anaesthetic. The anaesthetists' findings on the history and clinical examination of patients are often summarised in a more objective format, such as the American Society of Anesthesiologists (ASA) physical status grading system, which gives a score from 1 to 6 to denote the degree of risk of peri-operative mortality (Table I). Anaesthetists then order appropriate investigations to ascertain the risk associated with the surgery, and to guide any required pre-operative optimisation of function.2
HIV infection remains clinically latent for a variable length of time. Infected individuals may only present with signs or symptoms once they are already severely immunocompromised, and may appear clinically 'normal' despite marked levels of immune suppression.3 Our concern is that a patient who is clinically well on physical examination, with no features to prompt further investigation, may be HIV positive, with a significant level of immune compromise. The implications of this are unclear, as few studies have focused on this subgroup of patients in the peri-operative period.
We wished to investigate whether the pre-operative clinical condition of a patient correlates with subsequent laboratory testing for HIV infection and immune compromise. The primary objective was to determine the association between HIV infection (and the level of immune compromise in HIV-positive patients, as determined by the CD4 count) and preoperative physical status (determined by the ASA physical status grading). The secondary objective was to determine the prevalence of HIV in the total patient population and in subgroups of different patient characteristics, namely age, gender, type of surgery (obstetric or non-obstetric), urgency of surgery (elective or emergency) and nature of surgery (clean or septic) at CHBH. To our knowledge, no similar study has been published.
Methods
The study was conducted at CHBH. Permission was granted by the hospital superintendent and the study was approved by the regional Ethics Committee - the Committee for Research on Human Subjects (Medical) of the University of the Witwatersrand (protocol number M040230).
A sample population of 350 adult patients was selected. Patients <18 years of age and those presenting for procedures where an anaesthetist was not involved (e.g. local anaesthesia or conscious sedation administered by an assistant) were excluded. A daily list was compiled of all patients booked for elective and emergency procedures during the 24-hour period. One in every 3 of these was selected and added to a second list, which comprised the sample population. A trained counsellor gave pre-test counselling, and informed consent was obtained. Patients were sampled over a time period of 6 weeks, during December and January 2006, and sampling ended once 350 patients had consented.
All patients were interviewed and examined by the principal investigator. The ASA physical status grading was determined before knowing the HIV status of the patient. In patients with no other systemic illnesses, the ASA grading was as follows: ASA 1 - no signs of immune compromise or comorbid disease and no functional impairment; ASA 2, 3 or 4 - clinical signs of immune compromise or AIDS (e.g. oral candidiasis, generalised lymphadenopathy, generalised muscle wasting, peripheral neuropathy, systemic infections) graded according to their level of functional impairment. Patients known to be HIV positive, including those receiving highly active antiretroviral therapy (HAART), were also graded as ASA 2, 3 or 4, depending on their level of functional impairment. Patients with other systemic diseases were graded according to the functional impairment conferred on them by the combination of those diseases and any features of immune compromise.
Secondary data were recorded regarding their age group (18 - 29; 30 - 39; 40 - 49; 50 - 59; >60 years), gender and ASA physical status grading (1 - 5), type of surgery (obstetric or non-obstetric) they had been booked for, urgency of the procedure (elective or emergency) and nature of the surgery (clean or contaminated). The knowledge of HIV status was recorded.
Patients who did not know their HIV status had blood sampled for HIV testing and CD4 count. Patients known to be HIV positive had blood sampled for CD4 count only. Blood samples were sent for rapid HIV antibody testing and those that tested positive were sent for confirmatory HIV ELISA testing and the results recorded. Samples for CD4 count were only sent for testing for confirmed HIV-positive patients and the results were grouped as follows: <50; 50 - 199; 200 - 349; 350 - 499; >500 (cells/µl).
Patients were given their test results postoperatively with appropriate post-test counselling, unless they chose not to receive them. Patients who had tested HIV positive were referred to the Department of Infectious Diseases for ongoing management of their condition. Patients were not followed up postoperatively.
The data were analysed using the Stata statistical software package. The association between ASA physical status grading and HIV status and CD4 count (in those patients who tested HIV positive) was described. Logistic regression analysis and the Mantel-Haenszel combined odds ratio were used to adjust for the presence of confounding variables. The prevalence of HIV infection was determined in the total sample and in the subgroups, and these were compared using the chi-squared test, Fisher's exact test or the continuity correction.
Results
A total of 369 patients were approached for inclusion in the study. Nineteen patients (5.1%) did not give consent. Of the remaining 350 patients, 103 were confirmed or previously known to be HIV positive, giving an overall prevalence of 29.4% (p<0.0001).
The total sample distribution according to ASA grade and HIV status is shown in Table II. The classification of ASA grade was most affected by age, regardless of HIV status. Younger patients were more likely to be classified as ASA 1 or 2 than older patients (p<0.0001).

Within the HIV-positive group, the likelihood of being classified as ASA 1 or 2 (as opposed to being classified ASA 3 or 4) was analysed. Confounders were found to be the nature of surgery (clean or septic) and the urgency of surgery (elective or emergency). After adjusting for these, patients were more likely to be ASA 1 or 2 than ASA 3 or 4, with an adjusted odds ratio (OR) of 2.1 (p<0.05).
The distribution of data according to ASA grade and CD4 count in the HIV-positive group is shown in Table III. No patients met the criteria for classification as ASA 5 or 6. Patients were more likely to be ASA 1 or 2 than ASA 3 or 4 if their CD4 count was >200 cells/µl (crude OR 3.88, p<0.05). Of patients with CD4 counts <200 cells/µl (N=27), 21 (77.8%) were also classified as ASA 1 or 2, representing a significant majority (p<0.0001). Moreover, 3 patients with a CD4 count <50 cells/µl were also classified as ASA 1 or 2.

The prevalence of HIV in the different subgroups is shown in Table IV. Patients aged 30 - 39 years (43.0%) had the highest HIV prevalence; the lowest was in patients >60 years (7.7%); females had a higher prevalence of HIV than males (p<0.005); and patients undergoing obstetric procedures had a higher prevalence than those undergoing non-obstetric procedures (p<0.05). The nature of surgery (clean or septic) and the urgency of surgery (elective or emergency) revealed no significant differences in HIV prevalence.

Only 103 patients (29.4%) were aware of their HIV status. Of these, 38 (36.9%) were HIV positive, representing 10.9% of the total sample. There were HIV-negative and HIV-positive patients who chose not to learn their test results; they were encouraged to contact the principal investigator if they changed their mind.
Discussion
The prevalence of HIV infection in patients presenting for anaesthesia at CHBH is high (29.4%), is comparable to women presenting to antenatal clinics in South Africa (15.4 - 40.7%),4 is higher than the Nelson Mandela/HSRC Household Surveys' figures (10.8 - 11.4%),5,6 and is considerably higher than prevalence rates quoted for sub-Saharan Africa by the World Health Organization (7.2% in 2005).1
The ASA physical status grading system is widely used in clinical practice because it is simple and requires few, if any, special investigations. Patients graded as ASA 1 or 2 are generally considered to be in good health and fit for surgery and anaesthesia, and further investigations are often not deemed necessary, otherwise usually limited to very basic tests. However, patients graded as ASA 3 - 5 are usually re-assessed individually to create a management plan to best suit their clinical situation, and this often involves further special investigations.2
In this study, patients with HIV infection were more likely to be graded as ASA 1 or 2 than ASA 3 or 4 (adjusted OR 2.1). This is not surprising, considering the natural course of HIV infection. Infected individuals remain clinically latent until their viral load increases and their CD4 count drops, creating the clinical picture of AIDS. It was therefore expected that patients with CD4 counts >200 cells/µl would appear clinically well, and that patients with criteria for the diagnosis of AIDS (we used a CD4 count <200 cells/µl) would be severely functionally impaired, therefore being graded as ASA 3 - 5. Overall, this criterion was reflected - HIV-positive patients with CD4 counts >200 cells/µl were more likely to be graded as ASA 1 or 2 than patients with CD4 counts <200 cells/µl (OR 3.88). However, within the group of HIV-positive patients with CD4 counts <200 cells/µl, a significant majority (21 out of 27 (77.8%)) were still graded as having no or minimal functional impairment (ASA 1 or 2). This shows that patients with a confirmed diagnosis of AIDS, and therefore severe levels of immune compromise, may still be found to be 'fit for anaesthesia' by our usual clinical assessment. Some clinicians do not assign an ASA physical status grading based purely on functional status, as in our study, and might have graded patients with normal functional status as well as signs of immune compromise (e.g. oral candidiasis) as ASA 3. This remains a debatable issue.
The implications of these findings are twofold, especially in view of the results regarding patients' knowledge of their own HIV status (only 29.4% knew their status, and only 10.9% of the sample knew they were HIV positive).
Firstly, guidelines for pre-operative assessment and investigation indicated that patients who appear clinically well usually do not require further investigations before surgery.2 Our study indicates that in this population, with a high HIV prevalence rate, this practice will probably result in a number of patients with undiagnosed AIDS being missed on clinical assessment. What this means in practice remains to be established. For example, a patient with undiagnosed AIDS may harbour a cardiomyopathy, which may be subclinical under normal circumstances but may be a reason for a sudden, unexplained anaesthetic death, such as may occur following severe, intractable hypotension after spinal anaesthesia. There are few data regarding anaesthetic outcome measures in such patients. Literature regarding the immunosuppressive effects of anaesthesia (some techniques possibly conferring more effects than others7,8) may suggest cause for concern in this already immunodeficient group but is speculative and the effects remain to be conclusively shown.9 Surgical literature has implied that in certain scenarios (e.g. open colorectal surgery) patients with AIDS have an adverse clinical outcome10-2 and should be offered alternative management,13 although strict definitions of which groups are more at risk have not been provided.
Secondly, it is possible that, in the scenario of AIDS, clinical assessment may be insufficient to assess patients pre-operatively. In a setting with a high HIV prevalence, it may be necessary to find ways to increase the number of patients who are screened for HIV infection to enable clinicians to determine the level of immune compromise before surgery in HIV-positive patients and the need for further investigation.
Our secondary objective was to observe trends in other characteristics of the sample. Females, younger patients (especially aged 30 - 39 years) and patients presenting for obstetric procedures had significantly higher HIV infection rates than the others. These results were expected, as they follow similar trends in national survey findings.5 Importantly, even the group with the lowest risk for HIV infection (age >60 years) had an HIV prevalence rate of 7.7%, a significant proportion compared with global findings.1
Limitations of this study include: (i) It was not blinded. Investigators specifically looked for features of immune compromise in all patients, a few being oral candidiasis, melanonychia, muscle wasting and peripheral neuropathy. A blinded study might have had even more significant results, because many of these features are not routinely looked for during clinical assessment. (ii) The use of the ASA physical grading system as a judge of 'clinical wellness' may be criticised, as it is subjective. Criteria for each ASA physical status grading category were discussed in detail to minimise variability between investigators.
We investigated the pre-operative assessment of patients. Further investigation is warranted, particularly into the postoperative outcomes of patients with AIDS who undergo anaesthesia (whether anaesthetic, surgical or immunological), which would elicit valuable information pertaining to the needs of this group.
We are grateful to Mr E Musenge, Dr L Bocchino, Dr L Brannigan, Ms S Le Roux and Mrs J Scribante for their assistance, and the South African Society of Anaesthesiologists for funding.
References
1. World Health Organization. AIDS Epidemic Update, December 2005. Geneva: World Health Organization, 2005. www.who.int/hiv/epi-update2005_en.pdf (accessed 17 November 2006). [ Links ]
2. Practice advisory for preanesthesia evaluation: a report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology 2002; 96(2): 485-496. [ Links ]
3. Wilson DSN, Bekker L-G, Cotton M, Maartens G. Handbook of HIV Medicine. Cape Town: Oxford University Press Southern Africa, 2002: 1-60. [ Links ]
4. National HIV and syphilis sero-prevalence surveys of women attending public antenatal clinics in South Africa. www.doh.gov.za/docs (accessed 10 March 2006). [ Links ]
5. Nelson Mandela/HSRC Study of HIV/AIDS. South African National HIV Prevalence, Behavioural Risks and Mass Media Household Survey 2005. Cape Town: HSRC Press, 2005. [ Links ]
6. Nelson Mandela/HSRC Study of HIV/AIDS. South African National HIV Prevalence, Behavioural Risks and Mass Media Household Survey 2002. Cape Town: HSRC Press, 2002. [ Links ]
7. Schneemilch CE, Ittenson A, Ansorge S, Hachenberg T, Bank U. Effect of 2 anesthetic techniques on the postoperative proinflammatory and anti-inflammatory cytokine response and cellular immune function to minor surgery. J Clin Anesth 2005; 17(7): 517-527. [ Links ]
8. Volk T, Schenk M, Voigt K, Tohtz S, Putzier M, Kox WJ. Postoperative epidural anesthesia preserves lymphocyte, but not monocyte, immune function after major spine surgery. Anesth Analg 2004; 98(4): 1086-1092, table of contents. [ Links ]
9. Schneemilch CE, Schilling T, Bank U. Effects of general anaesthesia on inflammation. Best Pract Res Clin Anaesthesiol 2004; 18(3): 493-507. [ Links ]
10. van Marle JTL, Weir G, Botes K. Vascular disease in HIV/AIDS patients. S Afr Med J 2002; 92(12): 974-978. [ Links ]
11. Tran HS, Moncure M, Tarnoff M, et al. Predictors of operative outcome in patients with human immunodeficiency virus infection and acquired immunodeficiency syndrome. Am J Surg 2000; 180(3): 228-233. [ Links ]
12. Savioz D, Chilcott M, Ludwig C, et al. Preoperative counts of CD4 T-lymphocytes and early postoperative infective complications in HIV-positive patients. Eur J Surg 1998; 164(7): 483-487. [ Links ]
13. Sylla P, Kirman I, Whelan RL. Immunological advantages of advanced laparoscopy. Surg Clin North Am 2005; 85(1): 1-18, vii. [ Links ]
 Correspondence:
Correspondence:
P R Penfold
(prpenfold@mweb.co.za)
Accepted 27 May 2008













