Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.107 n.6 Pretoria Jun. 2017
https://doi.org/10.7196/samj.2017.v107i6.12391
IN PRACTICE
CLINICAL ALERT
Beware: The femoral haemodialysis catheter -a surgeon's perspective
T du ToitI; D ThomsonII; E MullerIII
IMB ChB, FCS, MMed, FEBS; Transplant Unit, Division of General Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
IIMB ChB, FCS, MMed, Cert Crit Care; Transplant Unit, Division of General Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
IIIMB ChB, FCS, MMed; Transplant Unit, Division of General Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
The ability to identify and address factors that threaten the optimal utilisation of donor organs is quintessential in obtaining satisfactory transplant outcomes. We share our concerns regarding the prolonged use of femoral haemodialysis catheters and its potential to jeopardise successful renal transplantation. Despite a paucity of literature on the topic, we review relevant aspects related to this pernicious form of vascular access and clarify its limited role in the modern haemodialysis unit, particularly in patients who are still considered for transplantation.
In South Africa, access to renal replacement therapy (RRT) and transplantation is limited, mainly owing to resource constraints. In the Western Cape Province, approximately half of the public sector patients with stage 5 chronic kidney disease are denied RRT.[1] Those who are accepted are typically good transplant candidates with favourable outcomes when transplanted (5-year patient and graft survival rates of 83.5% and 77.9%, respectively). Low national organ donation (1.4 per million population (pmp)) and renal transplantation rates (4.7 pmp)[1] demand optimal utilisation of this precious resource.
This article is based on recent adverse events encountered during renal transplantation at our institution, possibly associated with the prolonged use of femoral haemodialysis catheters (FHCs). Cumbersome dissection of target vasculature, prolonged anastomosis time and unpredictable venous outflow were some of the difficulties experienced, resulting in unsalvageable early graft thrombosis on two occasions.
Despite the anecdotal nature of these findings, we believe that the association with FHCs was not incidental. In the absence of prospective data, with glaring ethical concerns prohibiting further investigation by a randomised control trial, we attempt to answer three relevant questions by applying clinical experience and the best evidence at hand.
1. Are venous complications associated with upper-extremity haemodialysis catheters applicable to FHCs?
Prolonged catheterisation of the upper-extremity venous system may induce structural damage and (in its most extreme form) lead to central vein stenosis (CVS). Owing to its crippling effect on future vascular access, CVS has been extensively studied. In our opinion, in the absence of literature evaluating aetiopathological factors specific to lower-extremity venous stenosis, valuable parallels may be drawn from the substantial pool of data on CVS. However, one should recognise unique anatomical differences and how these may affect the development of venous complications.
The development of haemodialysis catheter-associated CVS is based on an interplay of mechanical forces, generated by dynamic mediastinal structures and turbulent flow.[2] Vein-wall thickening, proliferation of smooth-muscle cells and focal catheter attachment to the vein wall are consequences of prolonged catheter use.'31 A comparable interplay of mechanical forces applies to FHCs. Although dynamic mediastinal structures do not contribute to mechanical forces in the lower-limb setting, the mechanical implications of a relatively rigid intraluminal device positioned in an anatomically dynamic region have to be considered.
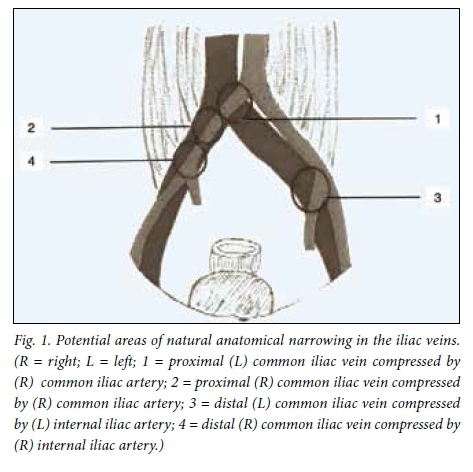
Areas of natural anatomical narrowing have been described and render the vessel wall vulnerable to direct mechanical trauma. In the upper extremities, these areas include the subclavian vein at the costoclavicular junction and the left brachiocephalic vein as it crosses a relatively fixed, pulsatile fulcrum of brachiocephalic artery and aorta.[4,5] Comparable areas in the lower-extremity venous system include both (but especially the left) common iliac veins where they are crossed by the right common iliac artery (Fig. 1).
Reports specifically evaluating the impact of FHCs on the surrounding vasculature are limited.[6,7] A retrospective study, including 24 patients receiving haemodialysis by way of a temporary FHC, investigated the frequency of post-catheterisation common femoral/ external iliac vein stenosis.[6] Magnetic resonance (MR) venography (comparable to conventional venography)[8] confirmed venous stenoses in 4 of the 14 patients (29%) with >14 catheter days. All stenoses observed were in the subgroup of patients with >30 catheter days. Comparatively, the reported stenosis rates with internal jugular and subclavian vein catheters are 10%[9] and 20 - 50%,[9-11] respectively.
In another study, 7 of 27 patients (26%) with tunnelled FHCs presented with ipsilateral lower-extremity swelling within 10 days of insertion. Deep-vein thromboses were ultrasonographically confirmed in all 7 cases.'121
2. What are the implications of prolonged FHC use, with specific reference to renal transplantation?
Several imaging modalities (including duplex ultrasound,[13,14] computed tomography venography and (3-D) MR venography'151) have been validated in the diagnosis and exclusion of post-catheterisation venous stenosis. However, exclusion of significant stenosis (accepted as >50%) does not necessarily predict successful transplantation. Once reperfused, the renal allograft will receive approximately 10 - 12% of the recipient's cardiac output. This equates to an increase in iliac vein outflow of approximately 550 mL/min in a 70 kg adult male.[16] In the presence of unrecognised upstream perivascular fibrosis and reduced venous compliance, a functional stenosis may only be unmasked upon reperfusion, potentially leading to allograft congestion and early renal vein thrombosis.
Successful transplantation contralateral to the side of suspected venous pathology has been described.[6] However, an important consideration is the physical length of the catheter and its position relative to the common iliac vein confluence (Fig. 2). Long-term (tunnelled) FHCs are often longer than their temporary (non-tunnelled) counterparts, therefore potentially compromising contralateral external iliac vein outflow should stenosis develop.

In patients with venous pathology precluding heterotopic renal transplantation, an orthotopic site may be considered. In the largest orthotopic renal transplant series to date (223 transplants over a 31-year period) excellent 1-, 10- and 20-year overall patient (92%, 78% and 63%) and graft (88%, 59% and 35%) survival were reported, with no difference in 20-year patient or graft survival compared with heterotopic transplants.[17] However, the procedure is technically demanding and associated with high surgical complication rates (66.7%) when performed infrequently.[18]
3. How should one approach the chronic haemodialysis patient in need of an FHC?
Preserving the likelihood of successful transplantation is key. FHCs should be reserved for cases where internal jugular vein catheterisation is unsuccessful or contraindicated, with catheter days restricted to a minimum. Early referral to an access surgeon allows sufficient time for preoperative planning and usually results in prompt creation of alternative access in the majority of patients.
Patients with bilateral CVS not amenable to endovenous intervention present a unique challenge. The optimal long-term solution is expedited renal transplantation, and this should be motivated for by the treating physician on the basis of precarious vascular access. Reassessment for peritoneal dialysis is often overlooked, and relative contraindications should not apply in the face of dwindling vascular access. Owing to generally uninspiring outcomes, lower-extremity arteriovenous (AV) fistulas/grafts should not be viewed as sustainable access, but rather as a 'bridge' to transplantation.[19] In our opinion, all the above options should be explored prior to insertion of a long-term FHC as definitive access.
Conclusion
The correlation between early graft thrombosis and prolonged FHC use cannot be scientifically proven at this time. However, retrospective reports suggest that the iliac veins are not exempt from the venous complications associated with upper-extremity haemodialysis catheters. Although successful transplantation is still likely, prolonged FHC use may result in avoidable surgical complexities that cannot be reliably predicted preoperatively. Early graft thrombosis, despite occurring rarely, is not only devastating to the recipient and surgeon involved, but may also impact on the patient awaiting a chronic dialysis slot.
We therefore strongly believe that FHC placement should be reserved for patients in whom internal jugular vein catheterisation was unsuccessful or is contraindicated. A proactive approach to establishing alternative dialysis access is required in an effort to limit femoral catheter days, especially in patients who are still considered for transplantation. Where upper-limb access options are not viable, expedited renal transplantation, peritoneal dialysis and lower-extremity AV fistulas/graft creation should all be considered prior to insertion of a long-term FHC as definitive access.
Transplant surgeons should be informed of all patients on the waiting list with current or previous catheters beyond the common iliac vein confluence (or within both external iliac veins) for more than 30 cumulative days, as difficult transplantation should be anticipated.
Acknowledgements. None.
Author contributions. All authors contributed to the conceptualisation process, with EM and DT involved with the proofreading of the manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Moosa MR, Kidd M. The dangers of rationing dialysis treatment: The dilemma facing a developing country. Kidney Int 2006;70(6):1107-1114. http://dx.doi.org/10.1038/sj.ki.5001750 [ Links ]
2. Hernandez D, Diaz F, Rufino M, et al. Subclavian vascular access stenosis in dialysis patients: Natural history and risk factors. J Am Soc Nephrol 1998;9(8):1507-1510. [ Links ]
3. Forauer AR, Theoharis C. Histologic changes in the human vein wall adjacent to indwelling central venous catheters. J Vasc Interv Radiol 2003;14(9):1163-1168. http://dx.doi.org/10.1097/01.RVI.0000086531.86489.4C [ Links ]
4. Yevzlin AS. Hemodialysis catheter-associated central venous stenosis. Semin Dial 2008;21(6):522-527. http://dx.doi.org/10.nn/j.1525-139X.2008.00496.x [ Links ]
5. Salik E, Daftary A, Tal MG. Three-dimensional anatomy of the left central veins: Implications for dialysis catheter placement. J Vasc Interv Radiol 2007;18(3):361-364. http://dx.doi.org/10.1016/).jvir.2006.12.721 [ Links ]
6. Weyde W, Badowski R, Krajewska M, et al. Femoral and iliac vein stenoses after prolonged femoral vein catheter insertion. Nephrol Dial Transplant 2004;19(6):1618-1621. http://dx.doi.org/10.1093/ndt/gfh192 [ Links ]
7. Hegarty J, Picton M, Chandlers N, et al. Iliac vein stenosis secondary to femoral catheter placement. Nephrol Dial Transplant 2001;16(7):1520-1521. https://doi.org/10.1093/ndt/16.7.1520 [ Links ]
8. Yoshizako T, Kazuro K, Kawumitsu H, Yoshikawa K. Two-dimensional time-of-flight MR venography: Assessment with detection of chronic deep venous thrombosis in combination with magnetization transfer contrast. J Comput Assist Tomogr 1996;20(6):957-964. [ Links ]
9. Barret N, Spencer S, Mclvor J, Brown EA. Subclavian stenosis: A major complication of subclavian dialysis catheters. Nephrol Dial Transplant 1988;3(4):423-425. [ Links ]
10. Clark DD, Albina JE, Chazan JA. Subclavian vein stenosis and thrombosis: A potential serious complication in chronic hemodialysis patients. Am J Kidney Dis 1990;15(3):265-268. https://doi.org/10.1016/S0272-6386(12)80772-4 [ Links ]
11. Schillinger F, Schillinger D, Montagnac R, Milcent T. Post-catheterisation vein stenosis in haemodialysis: Comparative angiographic study of 50 subclavian and 50 internal jugular accesses. Nephrol Dial Transplant 1991;6(10):722-724. https://doi.org/10.1093/ndt/6.10.722 [ Links ]
12. Maya ID, Allon M. Outcomes of tunneled femoral hemodialysis catheters: Comparison with internal jugular vein catheters. Kidney Int 2005;68(6):2886-2889. http://dx.doi.org/10.1111/j.1523-1755.2005.00762.x [ Links ]
13. Rose SC, Kinney TB, Bundens WP, et al. Importance of Doppler analysis of transmitted atrial waveforms prior to placement of central venous access catheters. J Vasc Interv Radiol 1998;9(6):927-934. https://doi.org/10.1016/S1051-0443(98)70424-5 [ Links ]
14. Patel MC, Berman LH, Moss HA, McPherson SJ. Subclavian and internal jugular veins at Doppler US: Abnormal cardiac pulsatility and respiratory phasicity as a predictor of complete central occlusion. Radiology 1999;211(2):579-583. http://dx.doi.org/10.1148/radiology.211.2.r99ma08579 [ Links ]
15. Paksoy Y, Gormus N, Tercan MA. Three-dimensional contrast-enhanced magnetic resonance angiography (3-D CE-MRA) in the evaluation of hemodialysis access complications, and the condition of central veins in patients who are candidates for hemodialysis access. J Nephrol 2004;17(1):57-65. [ Links ]
16. Carlström M, Wilcox CS, Arendshorst WJ. Physiol Rev 2015;95(2):405-511. http://dx.doi.org/10.1152/physrev.00042.2012 [ Links ]
17. Musquera M. Orthotopic kidney transplantation: An alternative surgical technique in selected patients. Eur Urol 2010;58(6):927-933. http://dx.doi.org/10.1016/j.eururo.2010.09.023 [ Links ]
18. Hevia V, Gómez V, Álvarez S, Díez-Nicolás V, Fernández A, Burgos FJ. Orthotopic kidney transplant: A valid surgical alternative for complex patients. Curr Urol Rep 2015;16(1):470. http://dx.doi.org/10.1007/s11934-014-0470-x [ Links ]
19. Aitken E, Jackson AJ, Kasthuri R, Kingsmore DB. Bilateral central vein stenosis: Options for dialysis access and renal replacement therapy when all upper extremity access possibilities have been lost. J Vasc Access 2014;15(6):466-473. http://dx.doi.org/10.5301/jva.5000268 [ Links ]
 Correspondence:
Correspondence:
T du Toit
dutoitjm@yahoo.com
Accepted 15 March 2017













