Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309Print version ISSN 1681-150X
SA orthop. j. vol.10 n.1 Centurion Jan. 2011
CLINICAL ARTICLE
Cervical PEEK cage standalone fusion - the issue of subsidence
RN DunnI; C PretoriusII
IMBChB(UCT), FCS(SA)Orth, MMed(Orth) Associate Professor and Head of Spinal Services: Groote Schuur Hospital, Division of Orthopaedic Surgery, University of Cape Town, Cape Town, South Africa
IIMBChB(Pret) Registrar, Department of Orthopaedic Surgery, University of Stellenbosch
Introduction
Anterior discectomy and interbody fusion is a well-accepted management option for the treatment of persistent cervical radiculopathy or myelopathy due to focal stenosis. The Smith-Robinson anterior approach1 utilises the plane between the sternocleidomastoid and neurovascular bundle laterally and the strap muscles, trachea and oesophagus medially to rapidly and bloodlessly expose the cervical spine. Following annulotomy, the offending disc material is removed and the canal and foramina cleared, thus decompressing the thecal sac and exiting nerve roots. Typically a fusion is performed to stabilise the segment, maintain foraminal height and the normal sagittal profile.
The Smith-Robinson fusion technique1 described in 1958 using tri-cortical anterior iliac crest autograft is the gold standard with excellent reported fusion rates and symptomatic resolution. The Cloward technique2 using a cylindrical graft was popular but is less frequently used now due to dangers related to reaming the cervical column and graft collapse.
With the use of uninstrumented autograft fusions, there is an incidence of graft displacement, subsidence and non-union1,3,4,5 especially if poor bone stock is used. With the age of instrumentation, anterior cervical plating was added. This brought its own problems. Plating requires increased longitudinal exposure, has the risk of adjacent disc violation by screws and may increase the rate of dysphagia due to plate prominence. Allograft iliac crest graft has been used with fusion rates approximating autograft.
More recently synthetic cages, initially titanium and more recently PEEK have been employed. PEEK has the advantage of biomechanical properties similar to bone, but more importantly to the clinician is its radiographic transparency facilitating postoperative fusion confirmation. Cages can be used with an adjunctive plate or as standalone devices. There is some concern regarding standalone use, especially as regards expulsion or migration.6
This study presents our experience with the use of standalone PEEK cervical interbody cages.
Methods
A retrospective review was performed on 34 consecutive patients undergoing standalone cervical interbody PEEK (polyetheretherketone) cage decompression and fusion. The Cornerstone® cage (Medtronic) was used in 31 cases and the Solis® (Stryker) in three patients. The surgery was performed by the senior author (RND) from September 2003 to December 2009.
Surgical indications were cervical radiculopathy unresponsive to medical care of a minimum of 6 weeks or established myelopathy. Pre-operative X-rays and MRI scans were performed to confirm the diagnosis. A right-sided Smith-Robinson approach was used. Caspar dis-tractor pins were used to open the disc space, especially posteriorly. The disc was removed and the decompression done. The thecal sac and appropriate proximal part of the roots were visualised. In the case of osteophytic pathology, this was burred away until decompression was satisfactory. The endplates were prepared to bleeding bone. The cage was sized with trials, releasing the distracter pins to confirm resistance to pull-out. Bone graft was harvested percutaneously with a tube from the iliac crest. This graft was packed into the selected cage. The cage was placed into the disc space under direct vision. The depth of insertion was confirmed with lateral fluoroscopy. The average skin-to-skin duration was 82 (30-165 ± 30.4) minutes with an expected significant difference between single level 75 (30-150 ± 24.4) and double level 132 (115-165 ± 22.5) surgery (p=0.01). The average blood loss was 65 ml (10-200 ± 44.9) with single level 59 ml (10-200 ± 39.7)and double level 112 ml (75-200 ± 59.5) (p=0.01).
Case notes were reviewed for presenting symptoms, patient age and diagnosis. Surgical parameters including duration of the surgery, blood loss, fusion level, cage size and complications were recorded.
Radiological parameters were assessed at fixed time points from pre-op to a maximum of 2 years in terms of kyphosis, cage migration and subsidence, as well as fusion. The lateral C2-7 angle was used for regional assessment and posterior body wall for the local angle. Disc height was measured directly as well as a ratio to the body width to correct for changes in X-ray magnification. The AP X-ray was assessed for lateral cage migration. Fusion was assessed as present if trabecular continuity and bone bridging across the disc space was present. Although planned follow-up is two years, once fusion was obtained and communicated to patients, they often failed to return as they perceived no benefit. This is borne out in our follow-up results explained later.
Of the 34 patients, 15 were male and 19 females. Twenty-four patients presented with a radiculopathy and 10 with myelopathy. The commonest radiculopathy was C6 (14) followed by C7 (7), C5 (2), C6 and C7 (1).
Eight patients underwent a C6/C7 fusion, 20 patients a C5/C6 fusion, one patient a C4/C5 fusion and one patient a C3/C4 fusion. Four patients received two-level fusions (Figure 1).
Results
The average age at surgery was 52.2 (26-78 ± 11.7) years, with a significant difference between the radiculopathy group at 49.7 (38-73 ± 10.8) years and the myelopathic group 58.3 (38-73 ± 10.8) years (p=0.02).
The most frequently used cage height was 6 mm (Figure 2).
Of the 34 patients, 26 had complete resolution of their presenting complaint, i.e. radicular pain or myelopathic features. The radiculopathy was typically resolved completely postoperatively with the myelopathy improving in a matter of weeks. This represented 22/24 (92%) radiculopathy patients and 4/10 (40%) myelopathy patients. The contrast in clinical success between the two groups was statistically significant (p=0.003).
Other than two intra-operative minor CSF leaks, there were no other recorded complications. These leaks were controlled with Duroseal application.
Thirty of the 34 patients had postoperative X-rays available for review.
The local angle improved from an average lordosis of 0.4º (-10 - +10 ± 3.5) to 2.7º (-15-10 ± 5.3) (p=0.02). This was maintained at 6 months? follow-up at 2.6º (-12-15 ± 7).
The disc height improved from 4.2 mm (2-6 ± 1.3) preop to 7.6 mm (4-10 ± 1.5) postop (p=0.000006). This was maintained at 3 and 6 months.
Subsidence was noted to occur in the postoperative period, postop 0 mm (0 - 0 ± 0), 3 months 1.5 mm (0 - 5 ± 1.34) (p=0.00000002), 6 months 2.1 mm (0 - 6 ± 1.7) (p=0.000015) and 1 year 0.8 mm (0 - 5 ± 1.5).
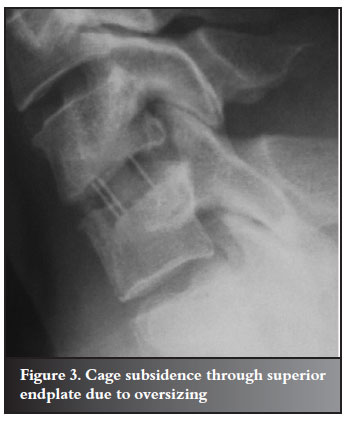
This apparent improvement between 6 and 12 months is incorrect and due to a diminishing number of longer-term X-rays available, thus representing a smaller group at 12 months than 6 months. With rapid symptom resolution and fusion confirmation, many patients do not see the need to return. An example of cage subsidence is demonstrated in Figure 3.
There was a trend to increased subsidence with increasing cage height (Figure 4).
No relationship between subsidence and clinical outcome was observed.
Fusion had occurred in 25/30 (83%) by 3 months, 26/30 by 6 months and 29/30 (92%) at final follow-up (Figure 5).

Surgery failed to relieve eight patients' symptoms. Of these, seven were radiographically fused. The remaining patient had a non-union at 1 year before defaulting final follow-up. Six of the eight were myelopathic. There was no cage migration or expulsion.
Discussion
Cervical surgery for radiculopathy in well-selected patients is usually successful as once the root is decompressed, the patient wakes without pain.3 The anterior approach popularised by Smith and Robinson is the mainstay of management due to easy patient positioning and intermuscular plane as compared to the posterior foraminotomies. The downside of the anterior approach is the requirement for fusion. There are proponents for discectomy alone, but this results in a spontaneous ankylosis with localised kyphosis. Thus most surgeons prefer an interbody fusion to maintain foraminal height and fuse the cervical spine in lordosis. Although intuitive and unproven in the human clinical setting, this is thought to minimise adjacent segment disease.5
Originally tricortical iliac crest autograft was used but had pseudarthrosis rates in excess of 10%, graft resorption with loss of sagittal correction, and risks of graft dislodgement.3,4
The use of a synthetic interbody cage reduces the iliac crest trauma. Allograft and synthetic bone replacement products are commercially available to completely avoid bone harvesting. In the reported cohort, percutaneous graft was harvested with a corer via an 8-10 mm stab incision. Local anaesthetic was infiltrated and it is the author's experience that patients tolerate this technique well and without complaint.
The cage cannot resorb, but there is an incidence of subsidence through the vertebral endplate. This has been shown above to increase over the first few postoperative months. There is seemingly a conflict in the reported data, as the disc height increased during the procedure and this increase was maintained - yet subsidence of the cage was noted. This may be explained by the associated simultaneous correction in lordosis which will affect disc height measurement. In addition, the disc height measurement was referenced to corners of the body, whereas the subsidence was in the central area of the body. Subsidence has been confirmed in another study by Kulkarni.6
In our study, this subsidence did not affect resolution of the patients' symptoms or the maintenance of the lordotic correction. There appeared to be more subsidence with the thicker cages. During this series, the author chose cage sizes on the basis of 'the bigger the better' as there was a concern about postop expulsion. An interference fit was thought to reduce the chance of migration and increase fusion rates. Frequently a mallet would be used to seat the cage posteriorly. As no migration/expulsion was experienced, the author is now less aggressive in terms of cage height.
Endplate integrity is paramount. There is the conflict of adequate preparation for fusion and not violating endplate strength. The cartilage is removed with a curette or osteophyte scraper, but caution should be exercised to avoid removing bone. This is sometimes difficult when the disc space is tight and posterolateral osteophytes need to be burred as this may require posterior endplate removal.
In double level surgeries, sizing should be performed serially, i.e. the second disc space trialed definitively once the first cage is in. If not, one often finds the second cage requires excessive persuasion to enter the disc space.
Subsidence has been shown to be reduced when combining posterior fixation in a study by Song et al.7 They focused on the management of kyphotic segments. In a neutral to lordotic cervical spine, the addition of a second approach seems likeoverkill, especially in the light that symptomatic improvement is not impaired by the presence of subsidence.
Conclusion
Cervical interbody fusion utilising a standalone PEEK cage is an effective method of achieving clinical symptom resolution in cervical radiculopathy. It achieves a high fusion rate without the graft-related complications reported with tricortical grafts.
However cage subsidence remains a concern and caution is recommended with endplate preparation and cage sizing, avoiding overstuffing.
References
1. Smith G, Robinson R. The treatment of cervical spine disorders by anterior removal of intervertebral disc interbody fusion. JBJS 1958;40A:607-24. [ Links ]
2. Cloward RB. The anterior approach for the removal ruptured cervical discs. J Neurosurg 1958;15:602-15. [ Links ]
3. Bohlman HH, Emery SE, Goodfellow DB. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow up of 122 patients. JBJS 1993;75A:1298-307. [ Links ]
4. White A, Southwick W, Deponte R. Relief of pain by anterior cervical-spine fusion for spondylosis. JBJS 1973;55A:525-34. [ Links ]
5. Goffin J, Geusens E, Vantomme N. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech 2004;17(2):79-85. [ Links ]
6. Kulkarni A, Hee H, Wong H. Solis cage (PEEK) for anterior cervical fusion: preliminary radiological results with emphasis on fusion and subsidence. The Spine Journal 2007;7:205-209. [ Links ]
7. Song K, Johnson J, Choi B. Anterior fusion alone compared with combined anterior and posterior fusion for the treatment of degenerative cervical kyphosis. JBJS 2010;92B:1548-52. [ Links ]
 Reprint requests:
Reprint requests:
Prof RN Dunn
Department of Orthopaedic Surgery. H49 OMB Groote Schuur Hospita
7925 Observatory Cape Town
Tel: (021) 4045387 Fax: 0866 715 294
Email: info@spinesurgery.co.za
No benefits of any form have been received from a commercial party relating directly or indirectly to the subjectof this article.













