Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Journal of Radiology
On-line version ISSN 2078-6778Print version ISSN 1027-202X
S. Afr. J. radiol. (Online) vol.23 n.1 Johannesburg 2019
https://doi.org/10.4102/sajr.v23i1.1729
REVIEW ARTICLE
Chest radiographs of cardiac devices (Part 1): Lines, tubes, non-cardiac medical devices and materials
Rishi P. Mathew; Timothy Alexander; Vimal Patel; Gavin Low
Department of Radiology and Diagnostic Imaging, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, Canada
ABSTRACT
Chest radiographs (CXRs) are the most common imaging investigations undertaken because of their value in evaluating the cardiorespiratory system. They play a vital role in intensive care units for evaluating the critically ill. It is therefore very common for the radiologist to encounter tubes, lines, medical devices and materials on a daily basis. It is important for the interpreting radiologist not only to identify these iatrogenic objects, but also to look for their accurate placement as well as for any complications related to their placement, which may be seen either on the immediate post-procedural CXR or on a follow-up CXR. In this article, we discussed and illustrated the routinely encountered tubes and lines that one may see on a CXR as well as some of their complications. In addition, we also provide a brief overview of other important non-cardiac medical devices and materials that may be seen on CXRs.
Keywords: Chest radiographs; endotracheal tube; tracheostomy tube; nasogastric tube; central venous catheter; Swan Ganz catheter; intercostal drainage tube.
Introduction
Among the various imaging modalities available for assessing the cardiothoracic system, the chest radiograph (CXR) is the most commonly used. In addition, the CXR is very useful in assessing the numerous tubes, lines, medical devices and materials, as well as for identifying any equipment-related complications. The American College of Radiology (ACR) recommends a CXR immediately after the placement of a medical tube, catheter or device, to check for malposition or for intra- or post-procedural-related complications. As any medical device has the potential for coiling, mispositioning, kinking or fracturing and malfunctioning, the complications that may ensue are often not immediately apparent clinically. Hence, it is of utmost importance to identify these on the immediate post-procedural CXR or follow-up CXRs for the physician or surgeon to replace or reposition these devices.1 The objective of this article is to provide a comprehensive review of the numerous tubes, lines and non-cardiac medical devices or materials that may be seen on CXRs, their appearance on CXRs and how to evaluate for their accurate placement, as well as to be aware of associated complications that need to be considered.
Tracheal and oesophageal tubes and lines
Endotracheal tube
The endotracheal (ET) tube is inserted for maintaining the patency of the airways or to provide airway support. The accurate positioning of the ET tube is assessed by calculating the distance of the tip of the ET tube from the carina. An ideal position would be 5 cm above the carina (Figure 1a) with the patient's head in a neutral position, taking into consideration that neck extension or flexion would lead to 2 cm of movement upwards or downwards. In cases where the carina is not visible on the CXR, the aortic 'knob' can be used as a useful landmark. The carina is just distal to the aortic arch, and if the ET tube is just above the aortic arch, it can be considered to be in a safe position midway between the vocal cords and the carina.2 If the carina is not visible an additional landmark that could be utilised is by confirming that the ET tip lies between the T2 and T4 vertebrae.3
A malpositioned ET tube (Figure 1b) is the most common complication associated with ET tube insertion. Complications associated with a wrongly placed cephalad ET tube include inefficient ventilation and distension of the stomach and vocal cord injury caused by the inflated cuff. Hence, the ET tube tip should be at least 3 cm caudal to the vocal cords. If the ET tube is advanced too caudally, the tube can selectively intubate one of the main bronchi, usually the right, leading to segmental or complete collapse of the lung. Accidental intubation of the oesophagus is a potentially fatal complication. In such cases, a frontal CXR may show the ET tube lateral to the tracheal air column and the identification of a column of air lateral to the trachea along with an overdistended stomach.4
Tracheostomy tube
Tracheostomy tubes (Figure 2) are inserted for long-term ventilation. Its distal end should be midway between the stoma and the carina at the level of third thoracic vertebra. When compared with the ET tube, the position of the tracheostomy tube is maintained with neck flexion and extension.
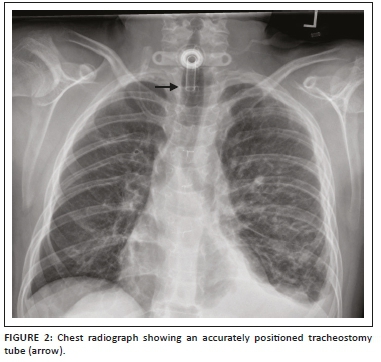
The width of the tube should not exceed two-thirds of the tracheal width, and the cuff should not distend the tracheal wall. Complications associated with tracheostomy tubes include subcutaneous emphysema, haematoma and pneumomediastinum. Granulation tissue formation and fibrosis at the site of the stoma can lead to tracheal stenosis.1,4
Nasogastric tube
Nasogastric (NG) tubes are frequently used for suction of stomach contents, administration of medication and for feeding. The NG tube has multiple side holes and a thin radiopaque marker line along one side, enabling it to be identified on a radiographic study (Figure 3a). The proximal side hole is indicated by a short break in this line. Both the upper side hole and tip should be located clearly below the gastroesophageal (GE) junction. An ideal position of the NG tube would be with its tip in the stomach caudal to gastric cardia or at least 10 cm distal to the GE junction.1,4 A malpositioned NG tube is the commonest complication and can lead to lung perforation, oesophageal perforation, pneumonia and pneumothorax.5,6
Dobhoff tubes are flexible tubes with a narrow bore measuring 4 mm in diameter for delivering enteral nutrition. Unlike NG tubes, suction cannot be applied to these tubes, making it useful only for feeding and delivery of drugs. These tubes provide two advantages over the NG tube1 because of their narrow bore; they are better tolerated by patients2, and the tubes enable post-pyloric feeding. These tubes are inserted into the stomach or duodenum with the aid of a guidewire through the nasal passage, which is then removed once the distal end of the tube is in an acceptable position. The distal end of the tube has a metallic end visible on a CXR. The gold standard for confirming an accurately inserted Dobhoff tube is by radiographic examination. Complications associated with these tubes include accidental insertion into the airway (Figure 3b), and if advanced further into the lungs may lead to trachea-pulmonary complications such as pneumothorax.7
Chest drainage or inter costal drainage tubes
An intercostal drainage tube, also called tube thoracostomy, is commonly inserted for pneumothorax, haemothorax, pleural effusion, and empyema. It also enables instilling antibiotics (after port pneumonectomy for empyema), fibrinolytics, saline and sclerosing agents (pleurodesis).
Both anteroposterior (AP) and lateral CXRs are required for optimal assessment of an intercostal drain (ICD) tube. Like the NG tube, an ICD tube also contains side holes that can be identified by the interruption of its radiopaque outline on a CXR. The side holes of the ICD tubes should be in the thoracic cavity and not in the chest wall or outside the chest. Some of the complications associated with ICD tubes that may be seen on CXRs include: malpositioning (commonest complication), tube kinking, subcutaneous emphysema, pneumothorax and retained catheter fragment.8 A properly placed tube for pneumothorax (Figure 4a) should orient antero-superiorly, and an adequately positioned tube for pleural fluid evacuation should be directed posterior-inferiorly. The numerous locations where the tube may be malpositioned include the interlobar fissure, lung parenchyma and subcutaneous soft tissues.9 There are several tubes available for thoracostomy and these include the traditional wide bore (>28 F) catheters and the newer popular pigtail catheters (10-14F) (Figure 4b) inserted by guide wires.10
Cardio-vascular lines on chest radiograph
Central venous catheter
A central venous catheter (CVC), also known as a central venous pressure (CVP) catheter or a central catheter or line, is a catheter (Figure 5a) that provides access for administering drugs or fluids, monitoring central venous or pulmonary artery pressure, monitoring central venous blood oxygen saturation, transvenous cardiac pacing, access for extracorporeal blood products and interventions. These catheters are usually inserted via the subclavian or internal jugular vein and less frequently via the femoral vein. A peripherally inserted central catheter (PICC) is a CVC of smaller calibre (Figure 5b) that is usually inserted via the antecubital vein and remains in place for months.2,11,12 Tunnelled CVCs (Figure 5c) are cuffed catheters that provide long-term intravenous access for a variety of purposes, which include parenteral nutrition, chemotherapy and haemodialysis. The commonest application for this CVC is for haemodialysis in patients with renal failure.13
Most clinicians prefer the CVC tip to be positioned at or just above the cavoatrial junction. As the cavoatrial junction may be difficult to identify on a CXR, the most commonly used and reproducible landmark is two vertebral body levels below the carina. An alternative landmark would be the reflection of the SVC contour with the right heart border and the point where the bronchus intermedius intersects the right heartborder.14 A lower placement is preferred for cannulations introduced from the left side. The various types of CVCs, potential contraindications and complications are shown in Table 112 and Figures 6 and 7.


Pulmonary artery catheter or Swan Ganz catheter
Pulmonary artery catheterisation involves inserting a catheter (Swan Ganz) through a central vein (mostly the subclavian or jugular vein and rarely through a femoral vein) into the right heart and finally into the pulmonary artery (Figure 8). Its function is to measure cardiac output, stroke volume, mixed venous oxygen saturation, intracardiac pressure and pulmonary wedge capillary pressure. An ideal location of the pulmonary artery catheter (PAC) tip would be in either the right or left pulmonary artery, not extending beyond the proximal interlobar artery, i.e. within 2 cm of the hilum. If the PAC tip extends beyond the large pulmonary arteries complications such pulmonary infarction or injury to small vessels, that is, pseudoaneurysm, can occur. A malpositioned PAC tip within the right ventricle increases the risk for ventricular arrhythmias and cardiac perforation.11,15,16 Other complications related to PAC insertion that may be seen on chest radiographs include pneumothorax, haematoma and catheter migration.16








Non-cardiac iatrogenic medical devices and materials
Medical devices and materials such as electrocardiogram (ECG) leads, ventilator tubing, syringes, clamps, temperature sensors, post-coronary artery bypass grafting (CABG) sternotomy wires, surgical clips, orthopaedic implants, gown snaps, etc. are commonly seen on CXRs. Because of its limited scope, we have not included cardiac devices in this article. However, there are other non-cardiac iatrogenic objects that can be seen on CXRs and these have been summarised in Table 2. Radiologists need to recognise them, be aware of their function and look for any related complications.
Conclusion
A variety of tubes, lines and medical devices may be seen on CXRs of patients admitted in a hospital. A thorough evaluation of these CXRs is important. Radiologists need to recognise these medical materials, assess them for accurate placement and look for abnormal radiographic presentations, which will enable them to inform the relevant physician or surgeon in a timely manner and help avoid potential consequences.
Acknowledgements
Competing interests
The authors have declared that no competing interests exist.
Author's contributions
R.P.M. was the project leader and wrote the manuscript. T.A. was the lead subject authority, supervised manuscript writing and helped acquire the images. V.P. did supervision of manuscript and helped acquire the images. G.L. did supervision of manuscript and helped acquire the images.
Ethical consideration
All ethical considerations have been taken into account. No patient identity or patient information has been revealed.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability statement
Data sharing is not applicable to this article as no new data were created or analysed in this study.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated agency of the authors.
References
1. Jain SN. A pictorial essay: Radiology of lines and tubes in the intensive care unit. Indian J Radiol Imaging. 2011;21(3):182-190. https://doi.org/0.4103/0971-3026.85365 [ Links ]
2. Hunter TB, Taljanovic MS, Tsau PH, et al. Medical devices of the chest. Radiographics. 2004;24(6):1725-1746. https://doi.org/10.1148/rg.246045031 [ Links ]
3. Goodman LR, Conrardy PA, Laing F, et al. Radiographic evaluation of endotracheal tube position. AJR Am J Roentgenol. 1976;127(3):433-434. https://doi.org/10.2214/ajr.127.3.433 [ Links ]
4. Godoy MC, Leitman BS, De Groot PM, et al. Chest radiography in the ICU: Part 1, Evaluation of airway, enteric, and pleural tubes. Am J Roentgenol. 2012;198(3):563-571. [ Links ]
5. Najafi M. Nasogastric tube insertion easily done: The SORT maneuver. Indian J Crit Care Med. 2016;20(8):492-493. https://doi.org/10.4103/0972-5229.188214 [ Links ]
6. Gachabayov M, Kubachev K, Neronov D. The importance of chest X-ray during nasogastric tube insertion. Int J Crit Illn Inj Sci. 2016;6(4):211-212. https://doi.org/10.4103/2229-5151.195453 [ Links ]
7. Abidali A, Mangram A, Shirah GR, et al. Bilateral Pneumothoraces in a Trauma Patient After Dobhoff Tube Insertion. Am J Case Rep. 2018;19:244-248. [ Links ]
8. Porcel JM. Chest tube drainage of the pleural space: A concise review for pulmonologists. Tuberc Respir Dis (Seoul). 2018;81(2):106-115. https://doi.org/10.4046/trd.2017.0107 [ Links ]
9. Taljanovic MS, Hunter TB, Freundlich IM, et al. Misplaced devices in the chest, abdomen, and pelvis: Part I. Semin Ultrasound CT MR. 2006;27(2):78-97. [ Links ]
10. Kuhajda I, Zarogoulidis K, Kougioumtzi I, et al. Tube thoracostomy; chest tube implantation and follow up. J Thorac Dis. 2014;6(Suppl 4):S470-S479. https://doi.org/10.3978/j.issn.2072-1439.2014.09.23 [ Links ]
11. Godoy MC, Leitman BS, De Groot PM, et al. Chest radiography in the ICU: Part 2, Evaluation of cardiovascular lines and other devices. AJR Am J Roentgenol. 2012;198(3):572-581. https://doi.org/10.2214/AJR.11.8124 [ Links ]
12. Smith RN, Nolan JP. Central venous catheters. BMJ. 2013;347:f6570. https://doi.org/10.1136/bmj.f6570 [ Links ]
13. Heberlein W. Principles of tunneled cuffed catheter placement. Tech Vasc Interv Radiol. 2011;14(4):192-197. https://doi.org/10.1053/j.tvir.2011.05.008 [ Links ]
14. Baskin KM, Jimenez RM, Cahill AM, et al. Cavoatrial junction and central venous anatomy: Implications for central venous access tip position. J Vasc Interv Radiol. 2008;19(3):359-365. https://doi.org/10.1016/j.jvir.2007.09.005 [ Links ]
15. Rajaram SS, Desai NK, Kalra A, et al. Pulmonary artery catheters for adult patients in intensive care. Cochrane Database Syst Rev. 2013;(2):Cd003408. https://doi.org/10.1002/14651858.CD003408.pub3 [ Links ]
16. Whitener S, Konoske R, Mark JB. Pulmonary artery catheter. Best Pract Res Clin Anaesthesiol. 2014;28(4):323-335. https://doi.org/10.1016/j.bpa.2014.08.003 [ Links ]
17. Gayer G, Petrovitch I, Jeffrey RB. Foreign objects encountered in the abdominal cavity at CT. Radiographics. 2011;31(2):409-428. https://doi.org/10.1148/rg.312105123 [ Links ]
18. Morani AC, Platt JF, Thomas AJ, et al. Hemostatic agents and tissue sealants: Potential mimics of abdominal abnormalities. AJR Am J Roentgenol. 2018;211(4):760-766. https://doi.org/10.2214/AJR.17.18991 [ Links ]
19. Harvey KL, Clark SE. A guide to breast implants for the non-breast specialist. Women's Health (Lond). 2016;12(6):533-537. https://doi.org/10.1177/1745505716687562 [ Links ]
20. Wallace AN, McConathy J, Menias CO, et al. Imaging evaluation of CSF shunts. AJR Am J Roentgenol. 2014;202(1):38-53. https://doi.org/10.2214/AJR.12.10270 [ Links ]
21. Jain A, Arora D, Mehta Y. Cardiac surgery in a patient with implanted vagal nerve stimulator. Ann Card Anaesth. 2018;21(1):57-59. https://doi.org/10.4103/aca.ACA_108_17 [ Links ]
22. Guinand A, Noble S, Frei A, et al. Extra-cardiac stimulators: What do cardiologists need to know? Europace. 2016;18(9):1299-1307. https://doi.org/10.1093/europace/euv453 [ Links ]
23. Sniderman KW. Noncoronary vascular stenting. Prog Cardiovasc Dis. 1996; 39(2):141-164. https://doi.org/10.1016/S0033-0620(96)80023-5 [ Links ]
24. Pron G, Common A, Simons M, et al. Interventional radiology and the use of metal stents in nonvascular clinical practice: A systematic overview. J Vasc Interv Radiol. 1999;10(5):613-628. [ Links ]
25. Rasmussen IC, Dahlstrand U, Sandblom G, et al. Fractures of self-expanding metallic stents in periampullary malignant biliary obstruction. Acta Radiol. 2009;50(7):730-737. https://doi.org/10.1080/02841850903039763 [ Links ]
26. Rasalkar DD, Paunipagar BK, Sonavane B. Migrating biliary stent with final destination at the ileocecal junction causing intestinal obstruction and obstructive biliopathy. Indian J Radiol Imaging. 2010;20(4):304-306. https://doi.org/10.4103/0971-3026.73535 [ Links ]
 Correspondence:
Correspondence:
Rishi Mathew
dr_rishimathew@yahoo.com
Received: 04 Mar. 2019
Accepted: 05 May 2019
Published: 29 July 2019













