Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562Print version ISSN 0011-8516
S. Afr. dent. j. vol.77 n.7 Johannesburg Aug. 2022
https://doi.org/10.17159/2519-0105/2022/v77no7a6
CASE REPORT
Pre-empting and preventing iatrogenic oral trauma: A case report
LM SykesI; B GrayII; V MostertIII; F Du PlessisIV
IBSc, BDS, MDent, IRENSA, Dip Forensic Path, Dip ESMEA; Head of Department of Prosthodontics, University of Pretoria. ORCID: 0000-0002-2002-6238
IIFinal year dental student, Department of Prosthodontics,Unversity of Pretoria
IIIBChD, MSc (dent), Dentist, Department of Prosthodontics, University of Pretoria
IVHDip Dent Tech, Senior dental technician, Department of Prosthodontics, University of Pretoria
ABSTRACT
In keeping with the principles of autonomy, beneficence, and non-maleficence, no dental treatment should be commenced prior to carrying out all the requisite preparatory stages. This includes a thorough initial assessment, establishing an accurate diagnosis, drawing up a list of possible treatment options, presenting these to the patient, and allowing them to make an autonomous and educated decision. This should be followed with the formulation of a structured and carefully considered treatment plan.This case illustrates a case of iatrogenically induced damage suffered by a patient where unplanned treatment was carried out with no consideration of the possible immediate, short term or long terms outcomes. It stresses the need for dentists to consider and pre-empt the consequences of their treatment (or lack there-of) and formulate the best possible plan for each patient. It also needs to be stressed that the proposed management plan must be informed by the principle of 'shared decision making' wherein the patient assumes part of the responsibility and accountability in the decisions taken. The ultimate aim of any plan must be to promote the best possible outcome for the patient (beneficence), and as far as possible prevent iatrogenically induced harm (non-maleficence).
Introduction
Dental treatment should not merely be structured to address the patient's immediate oral condition, but must also take a holistic approach and consider their future functional needs. With the exception of emergency procedures and immediate pain relief, no work should be commenced until the clinician has had the time to conduct a thorough clinical assessment and examination, and draw up a comprehensive, individually focused treatment plan1. This should include both immediate, short term and long term actions and objectives. Where possible the dentist should also try to pre-empt and prevent any discomfort, lack of function, psychosocial handicaps, and additional trauma during active therapy and after completion. This may entail provision of one or more interim prostheses that can function to prevent trauma to underlying sensitive structures, aid speech and mastication and serve as diagnostic aids for the definitive restorations 2. The following case report illustrates the importance of diagnosing a patient's presenting condition, determining their long-term dental plan, and simultaneously considering their interim status while awaiting healing and during active therapy.
Case Report
A 69 year old patient presented with seven remaining maxillary teeth (12, 11, 21, 22, 23, 24 and 25). These were all carious, chipped and slightly mobile. She had been wearing a maxillary metal based partial denture, which was now loose and ill fitting due to the fact that the 16, 17, 27 and 37 had been extracted a few months earlier. The opposing arch was edentulous posteriorly with severe attrition on the remaining anterior teeth (33 to 43). Oral hygiene status was poor, with all of the teeth having evident plaque deposits bucally, lingually and interdentally. There was a slight clicking in her left temporomandibular joint but no pain, deviation or limitation on opening were noted.
Her medical history revealed her to have high blood pressure for which she was receiving medication, as well as epilepsy, which she controlled with Epilem tablets (sodium valproate, 500mg taken daily). She also reported to suffer from anxiety and tension and was aware that she clenched and bruxed her teeth. This was evident from the worn down incisal edges and many chipped and sharp edges of her teeth. She had no allergies or any other systemic conditions of signifance. She was advised to have the remaining maxillary teeth extracted and an immediate maxillary complete denture opposing a mandibular Kennedy Class I denture fabricated.
Due to the sensitivity in the 12, and tongue irritation from the chipped edges, the patient requested that if she was to lose her remaining maxillary teeth, the extractions be done immediately, and to then have the dentures made after healing. Extractions were carried out that same day and due to the relative ease and lack of complications, no sutures or antibiotic coverage was deemed necessary. The patient returned a week later in severe pain. Intra-oral examination revealed severely traumatised and inflamed anterior maxillary ridge, poor healing of the sockets, pus exudates, and apparent dry sockets in the 21, 22, and 23 region (Figure 1).


It was evident that the patient had previously been chewing on her remaining anterior teeth and had continued to do so post extraction. This had led to the mandibular teeth now biting into the recent extraction sockets and causing considerable trauma to the ridge. The poor oral hygiene status of these teeth was no doubt a co-contributor to the resulting damage and infection.
Before any further treatment could be contemplated the sockets needed to be debrided and the tissues given time to heal. However the latter was not be possible if it was constantly being damaged and aggravated by her mandibular teeth. The dentist needed to devise some means of protection and shielding of the anterior maxilla until a denture could be fabricated.
The remaining teeth were scaled and polished and an impression was taken of the mandibular ridge. The cast was poured and a silicone mouth guard was made (Pro form mouth guard laminates, Keystone industries) which covered he remaining teeth and residual ridge. It was then further built up in the posterior edentulous areas with additional silicone creating 2 occlusal masticatory surfaces (Figure 3). The mouth guard was fitted into her mouth and adjusted until it was thick enough to allow her posterior maxillary ridges to come into contact with the rims while at the same time keeping the anterior mandibular teeth from biting into the anterior maxillary alveolar ridge. It was further reduced to ensure acceptable lip closure and patient comfort (Figure 4). All adjustments were made using visual assessment, aided by articulating paper and patient feedback.


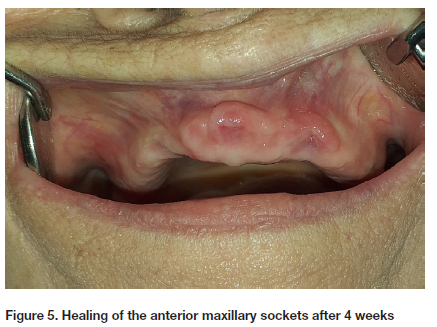
The patient was monitored for the next 4 weeks to assess the healing of the maxillary sockets, and ensure she maintained good hygiene prior to fabricating her definitive prostheses (Figures 5 and 6).

The patient was then provided with a new complete maxillary denture opposing a Kennedy Class I distal extension mandibular denture (Figures 7 and 8).


DISCUSSION
The long-term goal of comprehensive dental treatment should be the elimination of disease, creation of a healthy hard and soft tissue environment, provision of stable occlusion and function, and establishment of the best possible aesthetics (within reason)3. In order to achieve these goals, any intervention or treatment should be based on an accurate diagnosis followed by considered and well-structured treatment plan. The overarching proposal should not only focus on the tooth level, but must encompass a short, medium and long-term strategy that involves "treating the teeth within the context of the rest of the dentition, the masticatory system and the individual"4. It should also be holistic in nature, follow a predetermined plan, and be based on sound knowledge, communication, clinical skills, experience, current evidence and common sense4.
The following four steps are generally involved:
1. Collecting and collating relevant information.This
is obtained from the patient's history, their main complaints, the clinical examination, identification of coexistent diseases and conditions, and assessment of their attitude and desires. At this stage the clinician may be able to arrive at a tentative diagnosis, be aware of any systemic factors that could impact on the treatment or precautions that need to be taken, and have an idea about suitable treatment options4.
2. Establishing a diagnosis. An initial diagnosis may be possible based on the data collected, but the definitive plan often requires further specific investigations.
3. Consideration of treatment options.The mouth must be considered holistically including analysis of the dentition, periodontium, soft tissues, temporomandibular joints, occlusion, habits, oral hygiene and other possible confounding influences. The clinician needs to list and assess all options. These are generally based on dentist, patient, and oral factors. The former include their level of knowledge on current evidence based principles and best practice, clinical ability and available resources. Good clinical practice is based on academic knowledge, clinical competence, effective communication and ethical engagement 2. Patient related factors include the dentist: patient relationship, their desires and attitudes, their age, time and financial status, their ability to tolerate and maintain complex treatment, and anticipated oral hygiene practices. Dental considerations are the current oral hygiene status, degree of dental caries, tooth wear, periodontal disease, pulpal and endodontic status, functional occlusion, and appearance4.
4. Formulation of the treatment plan (with options)
The most appropriate treatment plan should be selected in order to "provide a masticatory system that is functionally adequate, free from disease and discomfort, aesthetically pleasing and acceptable to the patient"3.
The proposed plan should follow a logical progression that is convenient, appropriate and as stress-free as possible to both the clinician and patient. It should also make effective use of clinical time, provide the patient with sufficient information on issues such as time-frames, costs, expected outcomes, anticipated prognosis, possible complications, and possible contingency plans. The records must also be structured with enough detail to allow a colleague to take over therapy at any stage if needed 4.
Once the clinician is satisfied and confident that the treatment plan could meet the patient's needs and satisfy their desires, the final step is to "link the various components in a logical manner. A suggested treatment phase consists of: management of pain and emergencies and oral stabilization; prevention and disease control; followed by definitive restorative work; Review and occlusal analysis; definitive complex treatment and final maintenance and monitoring 4. Irrespective of what gain or loss a specific treatment offers, it is important that the patient is presented with a choice and the consequences explained 5.
In this case scenario it would appear that many of these recommended steps were not followed. Nor did the clinician consider or pre-empt the possible short and long term consequences of the immediate treatment, and failed to devise a plan to prevent these, while still addressing the patient's needs. Her history of bruxing, TMJ clicking and epilepsy should have alerted the dentist to her parafunctional habits, which would almost certainly continue after the extractions. She had already developed an altered masticatory pattern since the extraction of her posterior teeth the previous year in which her mandible moved antero- superiorly in order to chew on her only remaining teeth. One could have anticipated that this habit and altered mandibular posture would continue, but now her mandibular teeth would occlude with an edentulous anterior maxillary ridge and cause the trauma seen in this report. The poor oral hygiene and plaque was a further aggravating factor that was not addressed.
These teeth harboured plaque and bacteria that could have infected the opposing open sockets and should have been cleaned prior to the extractions. A more considered and pre-emptive treatment plan was needed at her initial consultation. Based on her initial panoramic radiograph (Figure 9) the two occluding posterior teeth (27 and 37) may have been retained6. These could have helped maintain the vertical dimension of occlusion and jaw posture, and provide retention and support for the interim partial dentures. At the same time she should have been educated on the importance of good oral hygiene and the need to maintain as many teeth as possible for bone preservation and future denture retention. Ideally she should also have had interim distal extension partial dentures fitted to prevent the posterior bite collapse, and her subsequent habit of chewing on her anterior teeth. "An interim prosthesis is designed to enhance the patient's aesthetics, stabilize the existing condition, and permit satisfactory masticatory function for a limited period of time"2. Such an interim appliance may also have reduced the strain on her TMJs, due to her clenching and bruxing habits. Provisional prostheses allow teeth and flanges to be added successively if and when needed, and can then be replaced with definitive dentures once the oral status has stabilised. This staggered transitional treatment approach is conservative, allows time for patient adjustment and adaptation, and permits the clinician to monitor oral hygiene and compliance. An occlusal splint on the other hand will not prevent the patient from bruxing but can help distribute masticatory forces more evenly7.
The poor oral hygiene and plaque was a further aggravating factor that was not addressed. These teeth harboured plaque and bacteria that could have infected the opposing open sockets and should have been cleaned prior to the extractions. A more considered and pre-emptive treatment plan was needed at her initial consultation. This may have helped prevent the need for all of the extractions and adverse consequences seen in the above case scenario. Based on her initial panoramic radiograph (Figure 9) the two occluding posterior teeth (27 and 37) may have been retained 6. These could have helped maintain the vertical dimension of occlusion and provide retention and support for the interim partial dentures. Oral hygiene education should have been reinforced at each visit to ensure she remained cognisant of the need to retain as many teeth as possible for bone preservation and future denture retention. Ideally she should also have had a distal extension partial denture fitted after her posterior mandibular teeth were extracted to prevent posterior bite collapse, and her habit of chewing on her anterior teeth7.
Alternatively, if the maxillary teeth were unsaveable, the treatment of choice should have been extraction with simultaneous provision of a complete immediate maxillary denture. These have many psychological, and functional advantages. The patient never has to be seen without teeth, the dentures restore speech, lip support and facial contour, and act as a splint / shield to protect the recent extraction sockets 6. It is important that clinicians explore all avenues to minimise changes that accompany the loss of teeth for the sake of the patient's emotional and physical well-being2.
CONCLUSIONS
In keeping with the principles of autonomy, beneficence, and non- maleficence,8,9 it is imperative that before commencing any treatment the dentist spends time on the initial preparatory stages. These include conducting a thorough initial assessment, establishing an accurate diagnosis, drawing up a list of possible treatment options, and presenting these to the patient. Thereafter they should help the patient make an autonomous and educated decision as to their preferred choice. This should be followed with the formulation of a structured and carefully considered treatment plan. Adherence to these basic initial steps could help improve patient understanding, compliance and satisfaction (beneficence), and more importantly, prevent iatrogenic oral trauma (non-maleficence).
REFERENCES
1. Benjamin SD. Oral diagnosis in the general practice. Compendium of continuing education in dentistry. 2011. Vol 32(2). Accessed at: https://www.aegisdentalnetwork.com/cced/special-issues/2011/09/oral-diagnosis-in-the-general-practice. Accessed on: 02-08-2021 [ Links ]
2. Mersel A. Immediate or transitional complete dentures: Gerodontic considerations. International dental journal. 2002. Aug; 2(4):298-303. [ Links ]
3. Cobb AC. Complete treatment planning: Meeting patients' needs. Inside dentistry. 2015. Vol 11. Issue 8. [ Links ]
4. Newsome P, Smales R., and Yip K. Oral diagnosis and treatment planning: Part 1. Introduction. Br Dent J. 2012. Vol213, No 1;15-20. [ Links ]
5. Ahmad I. Risk management in clinical practice. Part 5. Ethical considerations for dental enhancement procedures. Br Dent J 2010. Sep;209 (5):207-14. [ Links ]
6. Laney WR and Gibilisco, JA. Diagnosis and treatment planning in prosthodontics.1983. Ed Lea and Febiger; Philadelphia. Ch 9; pg208-215 [ Links ]
7. Dalal S, Shetty O, Mistry G. Occlusal splints. International J of Dental and Medical Sciences (IOSR-JDMS). 2018.52-3. [ Links ]
8. Day J and Stream S. Ethics in the Dental Office: Autonomy, beneficence, non-maleficence, and justice should guide your decisions. Dental Assistant. 2018. Jul 1;87 (4):8-9. [ Links ]
9. Beauchamp TI and Childress, JF. 2001. Principles of biomedical ethics. New York. Oxford University Press. [ Links ]
 Correspondence:
Correspondence:
Leanne Sykes
Head of Department of Prosthodontics
University of Pretoria.
Leanne.sykes@up.ac.za
Author contributions:
Leanne M Sykes: 60%
Bruce Gray 15%
Vanessa Mostert 15%
Francois Du Plessis 10%













