Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151Print version ISSN 0038-2361
S. Afr. j. surg. vol.54 n.4 Cape Town Nov. 2016
GUIDELINE
HIG (SA) Guidelines for the Management of Ventral Hernias
H BougardI, II; D CoolenIII; R de BeerIV; D FolscherV, VI; JC KloppersII, VII; MZ KotoVIII; GB ReimersIX; C SofianosX; R OoditVI, XI, XII
IHead Clinical Unit: Surgery, New Somerset Hospital, Cape Town, South Africa
IISenior Lecturer, University of Cape Town, Cape Town, South Africa
IIIPrivate Practice, Somerset West, South Africa
IVPrivate Practice, Bellville, South Africa
VPrivate Practice, George and Consultant Surgeon George Provincial Hospital, South Africa
VIHonorary Senior Lecturer, University of Cape Town, Cape Town, South Africa
VIIConsultant, Groote Schuur Hospital, Cape Town, South Africa
VIIIHead of Surgery, Sefako Makgatho Health Sciences University (SMU), South Africa
IXPrivate Practice, Pietermaritzburg, South Africa
XPrivate practice, Bedfordview, Johannesburg, South Africa
XIPrivate Practice, Cape Town, South Africa
XIIChair of the Hernia Interest Group, South Africa
Foreword
Ventral hernia repair is one of the most common general surgical procedures. The best opportunity for a successful outcome is the first repair. The last two decades has seen significant advances in surgical technique, types of mesh, fixation devices imaging techniques and the understanding of abdominal wall biomechanics. In addition, there has been a shift to a patient centered, evidenced based care and the importance of measuring outcomes increasingly recognized.
This has resulted in a significant shift in approach to hernia care worldwide. Despite these advances internationally, change has been slow in South Africa. It is clear that teaching, training and management in herniology need to be prioritized in South Africa. Care pathways need to shift to a tailored, patient-centered, evidence and consensus based paradigm and patient outcomes need to be measured.
The Hernia Interest Group of South Africa (HIG) established these guidelines with a view to creating a platform for change. These are the first national and international guidelines addressing both open and laparoscopic ventral hernia care. The HIG has presented objective, locally relevant guidelines that we believe will be useful to all surgeons, referring doctors, the health care industry and funders. The establishment of guidelines is a dynamic process and the intention is to update the guidelines every three years.
Ravi Oodit
Chair Hernia Interest Group of South Africa (HIG)
Executive Summary
• Careful attention should be paid to all modifiable risk factors which may prevent or reduce the incidence of incisional hernia.
• Patients with asymptomatic hernias should be offered a repair. This must be individualised based on patient risk, co-morbidities, life expectancy and type of hernia.
• All symptomatic hernias should be repaired unless there are contra-indications to surgery or anaesthesia.
• Emergency surgery should be conducted without delay, aiming for the simplest procedure with the lowest complication rate.
• Laparoscopic Ventral Hernia Surgery should be the approach of choice for patients with a BMI >35kg/m2,where technically feasible.
• Every incisional hernia requires a mesh repair.
• Primary ventral hernias with a defect > 2 cm require a mesh repair.
• Primary hernias < 2 cm in patients with risk factors for recurrence (obesity, concurrent hernia, recurrent hernia, concurrent diastasis or aneurysmal disease) require a mesh repair.
• Mesh placement for small hernias < 2cm has lower recurrence rate although slightly higher local wound complication rate than primary suture repair. However, these hernias can be suture repaired primarily.
• Open ventral hernia repair remains the standard, though the laparoscopic approach is a good alternative. The decision on approach should be based on patient wishes and surgical expertise.
• Uncomplicated extraperitoneal repairs should be performed with plain large pore polypropylene or polyester mesh.
• Intraperitoneal mesh repairs should be performed with a composite barrier mesh or strand coated anti-adhesion mesh.
• A minimum overlap of 5 cm before defect closure should be planned in all mesh repairs.
• Use of polypropylene mesh in contaminated wounds carries a high risk for septic complications and should be avoided.
• There is no evidence to support the routine use of biologic meshes. There may be a place for it in grade 3A and 3B wounds. The indications and clinical outcomes after use of biologics should be entered into registries or audited.
• All open incisional hernias should be repaired using mesh. The mesh should be placed in a retrorectus position. If not possible, the mesh should be placed in an underlay position.
• Careful inspection of the bowel pre, intra and post dissection should be carried out to avoid missed enterotomy. A high index of suspicion for enterotomy should be maintained throughout the postoperative course.
• Posterior Component Separation is the procedure of choice to obtain medial fascial advancement and the creation of a space for mesh placement.
• Patients presenting with a parastomal hernia should be advised to have an elective repair to avoid the complications accompanying emergency surgery.
• Patients having a permanent stoma fashioned should be offered prophylactic mesh placement.
• Rectus diastasis accompanied by a midline hernia should be repaired with a retrorectus mesh. In the absence of a concurrent hernia, repair of the diastasis should only be performed for compelling reasons.
• Complex abdominal wall reconstructions should be done in a unit with the necessary expertise.
• A failed repair increases the risk of subsequent failure by 50%.
• Informed consent should specifically include discussion on the use of mesh and the possibility of inadvertent enterotomy.
Introduction
Ventral hernia is one of the most common general surgical pathologies. An estimated 20 million patients with hernias are operated on worldwide every year, of which approximately 30% are ventral. An incisional hernia will develop in 10-15% of patients with an abdominal incision and the risk increases to up to 23% in those who develop surgical site infection.1,2 Incidence rates up to 69% have been reported in high-risk patients.3
Ventral hernia repairs are mostly elective (90%) procedures, but the repair methods are highly variable. Repair methods are often not based on current best practices and results can be disappointing.4 Few surgeons audit or record their outcomes outside of those countries with national registries.
Definition: Ventral hernias are defined as a defect of the fascia in the anterior abdominal wall with or without a bulge.5 Clinical presentation varies from small incidental defects to giant and complicated hernias with fistulas and viscera located outside the abdominal cavity covered only by peritoneum and skin (loss of domain).4 The symptoms range from minor cosmetic concerns to severe pain and life-threatening conditions such as bowel obstruction, incarceration, strangulation and perforation.
In establishing these guidelines, a first in South Africa, the Hernia Interest Group of South Africa, has set out to summarize and present best current evidence and provide a practical, patient-centred, tailored approach to this complex field.
SECTION A: CLASSIFICATION SYSTEMS
Grading of Recommendations
A simple grading system adopted from the Agency for Healthcare Research and Quality was employed.6
Category A: STRONG: There is good research-based evidence to support the recommendation
Category B: MODERATE: There is fair research-based evidence to support the recommendation
Category C: WEAK: The recommendation is based on expert opinion and panel consensus
Category X: AVOID: There is evidence of harm from this intervention
Classification of Ventral Hernias
Of the currently available classifications, we elected to use the European Hernia Society (EHS) classification as we deem this simple, practical and user friendly.7 It divides hernias into primary and incisional (secondary) and then further subdivides them by anatomical location and size. Incisional hernias are also categorised by recurrence in a binary fashion. (see Tables 1-4)
Primary hernias represent approximately two-thirds of all ventral hernias and are either congenital or acquired (approximately one-third). Incisional hernias are complications after previous surgery. The incidence of primary hernia repairs is reported as umbilical (71%), epigastric (25%), and other locations (4%).4,7
Incisional hernias develop in relation to incisions after laparotomy (89%), laparoscopy (5%), or in relation to a stoma (6%).4,7 Incisional hernias may also occur after penetrating abdominal trauma but there are only rare case reports in the literature.8 The incidence is suspected to be higher in the South African context.
The prevalence of umbilical hernias is 20-50% and epigastric hernias 2-4% of the adult population and it is estimated that only 0.1-0.5% of the umbilical hernias and 0.5-5% of epigastric hernias are repaired.9 Umbilical hernia repairs are predominantly performed in males aged 0-5 and 61-70 years, whereas epigastric hernia repairs are almost equally distributed by gender.10
The width of the hernia defect is defined as the greatest horizontal distance in centimetres (cm) between the lateral margins of the hernia defect on both sides. In the case of multiple hernia defects, the width is measured between the most laterally located margins of the most lateral defect on that side.
The length of the hernia defect is defined as the greatest vertical distance between the most cranial and the most caudal margin of the hernia defect. In case of multiple hernia defects from one incision, the length is between the cranial margin of the most cranial defect and the caudal margin of the most caudal defect. (see Figure 1)
Ventral Hernia Working Group Classification
In 2010, the Ventral Hernia Working Group11 published a grading system that attempted to stratify the risk of wound complications and recurrences in incisional hernias called surgical site occurrences (SSO) (see Table 5). In 2013, the group modified the classification based on new data, which more accurately defined outcomes in certain groups.12 The system is widely used to provide a framework for decision-making in incisional hernias, though many authors agree that it is only applicable to open surgery as risk factors for SSO are slightly different in the setting of Laparoscopic Ventral Hernia Surgery. Berger et al. have proposed a grading system for use in Laparoscopic Ventral Hernia Repair (LVHR) but it is not as yet widely adopted.12,13 It is also important to note that this grading excludes the type of hernia and operative technique. The presence of incarceration, strangulation, concomitant surgery, acute surgery and surgery related factors, such as operative time, extent of tissue dissection and use of drains, have not been included. A tailored or stratified approach to decision-making remains essential.
Informed Consent
In addition to the standard surgical consent, the following issues relevant to hernia surgery should be discussed:
• Options for treatment, including nonoperative care and laparoscopic vs open repair.
• The importance of preoperative optimization.
• The purpose and expected benefit of the intervention.
• The likelihood of short and long term success.
• The use of a mesh and its associated risks and benefits.
• The possibility of inadvertent enterotomy and its potential consequences and the treatment options in this setting.
• Other risks of the procedure including the possibility of conversion and or deferring repair.
SECTION B: INCIDENCE, AETIOLOGY AND PREVENTION
Incidence
Abdominal hernia repair is one of the most common operations in general surgery. The repair rate ranges from 10/100 000 population in the United Kingdom to 28 per 100 000 in the United States. No hernia repair data is available for South Africa.14
Abdominal operations are often complicated by incisional hernias. The commonly reported incidence varies from 2 to 20%.15 In high risk groups with long-term follow-up, this percentage may be as high as 69%.16 This variation is a result of some hernias only becoming evident many years after the initial operation.17 One in four men and one in fifty women will need surgery for an incisional hernia during their lifetime.18 The numbers of incisional hernias requiring emergency repair have been increasing. Morbidity and mortality in emergency cases is disproportionately high (23.6% morbidity and 4.9% mortality have been described).19
Most abdominal surgery is still performed by laparotomy in South Africa. The incidence of incisional hernia after laparotomy is 14 fold higher than after laparoscopy (9.9% compared to 0.7%)20
Hernia aetiology
Any injury or incision to the abdominal wall could lead to a hernia. Surgical technique and wound infection are considered the most important preventable causes of an incisional hernia.21 Many patient-related risk factors have been implicated.
Surgical site infections (SSI) are independent risk factors that significantly increase the risk of incisional hernias.22 Other factors are male gender, obesity,23 old age,24 diabetes mellitus, jaundice,22,23,25 anaemia, the use of vasopressor drugs,26 smoking,27 postoperative respiratory failure, aneurysmal disease, malnutrition, steroids, kidney failure, malignancy,21 abdominal distention,28 postoperative peritonitis,29 and multiple operations through the same incision.25 Chronic Obstructive Pulmonary Disease (COPD), benign prostatic hypertrophy, constipation and ascites increase the intra-abdominal pressure, increasing the risk of incisional hernias, but they are not considered independent risk factors.20 Diastasis of the rectus muscles also predisposes to an incisional hernia.15,30,31
Prevention of Incisional Hernias
Paramedian32 and transverse incisions33 are associated with a lower rate of incisional hernias compared to midline incisions. A statistically significant increase of incisional hernias after midline incision compared to transverse incision was reported at a Cochrane review in 2005 by Brown et al.33 The comparison of midline incisions to off-midline incisions also showed the same results. The incidence of incisional hernia was much higher with the midline incision (17.6% vs. 0%; P = 0.0002).34 Midline abdominal approaches should be avoided whenever feasible.
Careful attention should be paid to other strategies known to reduce surgical site infections (SSI). Measures known to reduce SSI may also lead to decreased incisional hernia incidence. These include prophylactic antibiotics, anti-bacterial sutures, wound-protectors, and care bundles.
Risk estimation scores to compare outcomes have been used in many surgical areas. The P-POSSUM risk assessment system (Physiological and Operative Severity Score for the enumeration of Morbidity and Mortality) can be used in both elective and emergency general surgical conditions, is easy to use and is freely available as an online calculator.35
Recommendation: The surgeon should be aware of the factors which increase the risk of surgical site infection rates and employ all available strategies to reduce the risk (Grade: Strong).
Wound Closure
A large number of studies have shown that good suture technique is extremely important to prevent wound complications, SSI, dehiscence and hernias.36
There is now level 1 evidence37 recommending that for optimal midline abdominal incision closure:36
• Use a slowly absorbable or non-absorbable monofilament suture preferably a 2/0 mounted on a small needle.
• Use a one-layer, continuous closure, taking only the aponeurosis, 5-8 mm from the wound edge, 4-5 mm apart. Include the peritoneum in each bite.
• Use self-locking anchor knots.
• Preserve the fascial edges of the rectus muscle by clearing a 2-4 cm space along the Linea Alba.38
Despite the evidence, most surgeons use a running suture technique with large, widely-spaced bites to close their midline incisions.16 A number of new closure techniques such as elastic sutures and mesh sutures are being trialled.38
Mesh Augmentation: There are 6 published RCTs on mesh augmentation for midline laparotomy closure. In high risk groups such as obese patients, those with previous hernias, and patients with aneurysmal disease, the risk reduction is very significant with a 1.5% incisional hernia rate in the mesh augmentation group vs 35.9% in the suture alone group (relative risk 0.17).36,39,40 It is now widely accepted that mesh should be used to augment all permanent stoma sites.41,42
Trocar Site Hernias: A systematic review of trocar site hernias43 reports an incidence of 0.5%. Risk factors for the development of port site hernia included use of 12 mm ports, pyramidal trocars and long duration of surgery. BMI and old age are patient-related risk factors. Interestingly, this review by Swank does not support the long held notion published in 2004 by Tonouchi that 10 mm port sites require suture closure as it makes no appreciable difference to the incidence of port site hernias.44
Trocar site hernias (TSH) are mainly located in the umbilical area. Repair rates for TSH are recorded as 1.35% in a series from the Danish Hernia Register.42 One in six repairs are performed as an emergency.
In an RCT published by Armananzas et al. it is suggested that all umbilical port sites in high risk patients are prophylactically closed with mesh.45
Recommendation: All midline laparotomies should be closed with non-absorbable or long-term absorbable sutures with a small bite continuous technique achieving a wound to suture length ratio of at least 4:1. The closure should be en masse and secured with self-locking knots. Prophylactic mesh should be considered in high risk patients (Grade: Strong).
SECTION C: INDICATIONS FOR SURGERY
Management decision-making for ventral hernias is complex and multifactorial. A tailored approach aims for the most appropriate operative strategy in an optimised patient, by a suitably experienced surgeon.
Acuity of presentation
Elective Asymptomatic Hernias: The natural history of ventral hernias is not well documented and it is common practice for most hernias to be surgically managed.46-48 The Danish database suggests that 10% of patients with asymptomatic hernias develop complications.42 Data is awaited from the Alliance Working for Antibiotic Resistance Education (AWARE) trial looking at whether patients with few symptoms will benefit from surgical management.49
Factors to consider:
• Umbilical hernias complicate 5 times more often than other ventral hernias.42,50
• The mortality and morbidity related to emergency hernia repair is very high - up to 45% morbidity51 and 25% mortality.50
• 33-78% of patients with an asymptomatic hernia will develop symptoms over the following 10 years.52
• 5-15% of hernias incarcerate.42,53
• 2.4% of hernias strangulate.53-55
• A failed repair increases the risk of subsequent failure by 50%. The first opportunity is the best opportunity.56
Recommendation: Patients with asymptomatic hernias should be offered repair. This must be individualised based on patient risk, co-morbidities, life expectancy and type of hernia (Grade: Strong).
Elective Symptomatic Hernia: Symptoms may include pain, discomfort, skin complications, irreducibility, or intermittent intestinal obstruction. All symptomatic hernias should be repaired if the patient has a life expectancy exceeding 2 years and there are no contraindications to general anaesthesia.57 Symptoms are considered a risk for the development of complications.
Recommendation: All symptomatic hernias should be repaired unless there are contra-indications to surgery or anaesthesia. (Grade: Strong).
Emergency hernia repair: Emergency indications for surgery are bowel obstruction, strangulation and perforation. Mortality and morbidity are disproportionately high (up to 50% in some studies).18,24,28 Clinical indicators of sepsis and ischaemia are not reliable and all patients with bowel obstruction from a hernia should be managed as an emergency.51,57,58
Recommendation: Emergency surgery should be conducted without delay, aiming for the simplest procedure with the lowest complication rate (Grade: Strong).
Surgical expertise
Outcomes in surgery are linked to both the experience of the surgeon and the volume of cases performed on an annual basis. This fact is documented in many surgical domains.59 The typical learning curve for a surgical procedure appears to be magnified in the learning of laparoscopic hernia surgery. The learning curve is longer for inguinal hernia surgery than for ventral hernia surgery.60,61
Recurrence rates and incidence of chronic pain are reduced in high volume units. The international trend is towards referral to centres of excellence for patients with complex hernias. The German Hernia Society stratifies centres into groups based on the volume of cases per annum and the extent of participation in the scientific community.62 Volume does not always equate to good outcome and objective outcomes are the best gauge of competency. South African surgeons need to consider and debate the merits of a national registry, specialist high volume hernia centres and/or audit systems.
Recommendation: Simple hernia surgery can be performed by a surgeon trained in hernia surgery and performing the procedure regularly. Complex hernias such as high risk patients, where there is loss of domain and recurrent hernias, should be performed only in units where significant numbers of these cases are performed and the expertise exists. The HIG offers training programs in hernia surgery for surgeons to improve skills (Grade: Moderate).
Obesity and ventral hernia surgery
Obesity is a risk factor for the occurrence of incisional hernias as well as for recurrence after repair. The reasons are multifactorial and are related to poor vascularisation of tissues, impaired wound healing, intra-abdominal pressure and impaired bio-mechanics.63 It is also a risk factor for the development of wound and mesh related complications in open ventral hernia repair.64,65 In obese patients (BMI > 35), laparoscopic repair reduces wound complications, other morbidity and the rate of recurrence.66,67 In a more recent long term follow-up, there was a trend to decreased recurrence and complications in the laparoscopic group but this was not statistically significant.68 A review of the > 47 000 patients in the USA National Inpatient Sample for 2008 and 2009 showed lower complication rate, length of stay (LOS) and cost in the laparoscopic group.69 This was confirmed for all BMI classes > 30 in an even larger review looking at the period 2009-2012.65 Although the National Surgical Quality Improvement Program (NSQIP) controls for risk factors, it does not control for surgical expertise, and is by nature still retrospective. In obese patients with BMI > 40 64,70 and > 35,71 laparoscopic repair offers comparable complication and recurrence rates to non-obese patients in expert hands, and decreased compared to published literature for the open repair. No RCTs looking specifically at the obese population are available.
Recommendation: Where technically feasible laparoscopic ventral hernia surgery should be the approach of choice for patients with BMI >35kg/m2 (Grade: Strong).
Should laparoscopic repair be used for incarcerated and strangulated hernias?
In incarcerated or strangulated ventral hernia, no level one evidence is available to guide the approach. Data from the American College of Surgeons NSQIP suggests a 5 fold decrease in superficial and deep SSI if the laparoscopic approach is used, combined with a slight advantage in LOS. The laparoscopic operation took 15 minutes longer on average.72
Recommendation: Laparoscopic repair may be employed in the setting of incarcerated or strangulated hernias. The risk reduction in SSI rates is noted though the surgeon's experience will dictate the approach (Grade: Moderate).
Concurrent umbilical repair during other procedures
The surgeon needs to take the size and complexity of the hernia, the risk of infection, the patient comorbidity and the patient's wishes into account when deciding on combining surgical procedures.
Laparoscopic Cholecystectomy: Umbilical hernias occur in approximately 8% of patients undergoing laparoscopic cholecystectomy.73 Raj et al. retrospectively looked at 246 combined procedures, either laparoscopic cholecystectomy or hysterectomy combined with mesh repair of incisional hernia.74 They found only 2 mesh infections and 2 recurrences and concluded that combined procedures are safe in "centres with adequate experience in management of laparoscopic ventral hernia repairs and by experienced laparoscopic surgeons." Mesh repair has the lowest recurrence rate. There is conflicting evidence about wound complication rates, but concurrent mesh repair appears to be safe and to carry no significant risks of wound complications. 73,75
Recommendation: Concurrent umbilical hernia repair should be performed during laparoscopic cholecystectomy (Grade: Moderate).
Inguinal Hernia: Concurrent laparoscopic hernia repair can be performed together with an open hernia repair of the umbilical defect. The principles for both repairs remain the same. Either totally extraperitoneal (TEP) or transabdominal preperitoneal (TAPP) can be safely performed followed by umbilical repair. Due to the high risk of recurrence the repair should be performed with mesh.
Recommendation: Umbilical Hernia Repair with mesh should be considered as a concurrent procedure when performing laparoscopic groin hernia repair (Grade: Weak).
Laparoscopic Bariatric Surgery: In bariatric surgery specifically, it appears that concomitant repair of incisional hernia with the primary bariatric procedure may be safe, with acceptable complication and recurrence rates.76 However, this is all anecdotal and case review data, and no high quality evidence exists.77
Recommendation: Concomitant repair of an incisional or ventral hernia could be considered as a single stage procedure during bariatric surgery (Grade: Moderate).
Umbilical hernia repair with ascites
Umbilical hernias occur in 20% of patients with liver cirrhosis complicated by ascites.78 Historically, mortality rates and hernia recurrence in patients with cirrhosis were prohibitively high and the accepted strategy was to reserve surgery for patients with a complication (incarceration, skin erosion and rupture). In the last decade the medical care of cirrhotic patients has improved and it has been shown that elective hernia repair is associated with fewer complications and may reduce overall mortality.79-82
Contraindications to elective surgery include acute liver failure, acute viral hepatitis and acute alcoholic hepatitis. Refractory ascites is associated with poor wound healing, infection and hernia recurrence. Perioperative control of the ascites is critical to a successful outcome.83 The timing of the hernia repair in liver transplant candidates should be made in conjunction with the transplant team.
A recent trial randomised patients with Child-Pugh A and B cirrhosis to either tissue or mesh repair. There was a non-significant increase in surgical site infection in the mesh group, but none needed removal of the mesh. On six month follow up, 14% of the tissue repair patients had recurrence compared to 3% in the mesh group. Permanent mesh can be used in complicated hernias in cirrhotic patients with minimal wound-related morbidity and a significantly reduced rate of recurrence.84
Recommendation: In patients with liver disease, an early elective mesh repair of umbilical hernia is encouraged. Preoperative control of ascites is especially critical to a successful outcome (Grade: Moderate).
Fertility and Pregnancy
Most surgeons are reluctant to place an Intra-peritoneal Onlay Mesh (IPOM) in fertile women wishing to conceive. There is concern about adhesion formation after intraperitoneal mesh placement, though there is a paucity of data on the topic.
Schoenmaeckers et al. report on a series of 8 women who safely carried to term and delivered without complications after mesh repair of a ventral/ incisional hernia.85 There is limited data and no conclusions can be drawn.
Hernias, particularly umbilical hernias, commonly become symptomatic during pregnancy and can be especially troublesome in the first trimester. However, the complication rates are very low and we advocate waiting until term.
If the baby is to be delivered by Caesarean section, it is often feasible to perform a concurrent repair taking advantage of the concomitant tissue expansion at the time of the caesarean. There is limited data that mesh placement is safe and that LOS and complication rates are not increased.86 If born by normal vertex delivery (NVD) the safest is to offer delayed repair.87
Recommendation: Perform a retro-rectus mesh hernia repair. Avoid intraperitoneal mesh placement in women wishing to conceive (Grade: Weak). Mesh repair can be performed at the time of Caesarean Section (Grade: Moderate).
Future abdominal surgery
Planned future surgery does not preclude mesh-placement. Every precaution should be taken to avoid adhesion formation. Should laparotomy be indicated after mesh repair, care should be taken on entry into the peritoneal space.88 It is important to re-suture the mesh on closure with non-absorbable suture material and to consider further mesh reinforcement if the fascia or mesh is incomplete.26
SECTION D: PERIOPERATIVE MANAGEMENT
Management of Risk Factors
Preoperative preparation should focus on rehabilitation. Risk factors such as smoking, diabetes, obesity, steroid use, HIV and other immunosuppression should be addressed prior to elective surgery, in order to optimise outcomes after hernia repair. Tools such as the P-POSSUM and CeDAR risk scoring systems (available as an app) are useful to determine implications of risk modification strategies.35,89
• Cessation of smoking for at least 4 weeks prior to surgery.90
• Optimising glycaemic control is important.91,92 A preoperative target HbA1c less than 7% is recommended.90 It is beneficial to keep the blood glucose normal during the first 24 hours after surgery.90
• Repair of incisional hernias in obese patients is associated with increased recurrence rates.93 Patients with BMI over 50 should not have an elective herniorrhaphy.
• Weight loss before surgery is strongly recommended in obese patients with a BMI greater than 35. Hernia repair preceded by physician monitored medical weight loss, concomitant hernia repair with weight loss surgery, or weight loss surgery staged prior to or after hernia repair are all viable options to approach this problem.77
• Adequately treat preoperative infections before surgery.94
• In HIV positive patients, the overall health, particularly the presence or absence of organ failure, and nutritional state (albumin < 2.5 g/dL) have been found to be more reliable predictors of surgical outcome than CD4 count or viral load in HIV-infected patients. It is recommended by the New York State Department of Health AIDS Institute that ART be optimised preoperatively.
• Hair removal from the operative site: if required, clipping of hair immediately before the operation is preferable.94
• Preoperative showers or antiseptic wash is not required for patients who are not carriers of methicillin resistant staphylococcus aureus (MRSA).94
Recommendation: Care should be taken to optimise the patient both medically and surgically preoperatively in order to ensure the best surgical and anaesthetic outcome (Grade: Strong).
Antibiotic prophylaxis
The clinical practice guidelines for antimicrobial prophylaxis recommend that a single dose of a first generation cephalosporin be administered within 60 minutes before skin incision.95 An MRSA carrier should have a single preoperative dose of vancomycin prior to surgery. Vancomycin should be administered within 120 minutes before surgery, because of its prolonged infusion time. As an adjuvant, intranasal mupirocin and chlorhexidine baths can be used. Consider guidelines from the local antibiotic stewardship committee. If a patient is allergic to beta-lactams, alternative antibiotics are clindamycin or vancomycin.95
The antibiotic dose should be repeated if the surgical procedure continues beyond 4 hours96 or there is significant blood loss (> 1.5 litres).95
There is no evidence to support continuing antibiotic prophylaxis in patients with drains and catheters.95 Recommendation: Single dose preoperative prophylactic antibiotic should be administered (Grade: Strong).
DVT/ VTE prophylaxis
Pulmonary embolism is a major cause of morbidity and mortality in surgical patients.
The presence of risk factors in a patient should be taken into consideration before giving thromboembolic prophylaxis.46 These risk factors should be considered when assessing a patient's risk in developing venous thrombo embolism (VTE) and could be patient-related and procedure-related.97
Deep venous thrombosis (DVT) prevalence in general surgical patients is 15-40%.97 Patient-related risk factors are: age > 60 years, history of VTE, immobility, underlying malignancies, pregnancy, oestrogen therapy, obesity, hereditary thrombophilic state, inflammatory bowel disease, HIV/AIDS, auto-immune diseases including antiphospholipid syndrome.97 Procedure related factors are duration of the procedure, degree of tissue damage, and degree of immobility.97
Laparoscopic repair is considered to be associated with lower risk of thromboembolic complications.98
Principles:
• Low-risk procedures (minor surgery) with no patient-related risk factors: No specific prophylaxis is required; early mobilisation is recommended.97
• Higher-risk procedures (major surgery) with no patient-related risk factors OR low-risk procedures with additional patient-related risk factors97: enoxaparin 40 mg sc (subcutaneous) daily or, dalteparin 0.2 ml sc daily, or nadroparin 0.3 ml. Prophylaxis can be given 12 hours before surgery and then once daily thereafter. Nadroparin is given sc 2 hours preoperatively and 8 hours after surgery, followed by 0.3 ml daily for 7 days. Intermittent compression devices can be used if there is a high risk of haemorrhage.
• Higher-risk procedures (major surgery) with additional patient-related risk factors [34]: enoxaparin 40 mg sc daily or, dalteparin 0.2 ml sc daily, or nadroparin 0.3 ml. Prophylaxis can be given 12 hours before surgery and then once daily thereafter. Nadroparin 0.3 ml is given sc 2 hours preoperatively and 8 hours after surgery, followed by 0.3 ml daily for 7 days. Additional pneumatic compression is advised.97
Timing of prophylaxis97: Prophylaxis can be given 12 hours before surgery. There are data indicating that starting prophylaxis 6-12 hours postoperatively is adequate, provided there is no active bleeding. The new oral anticoagulants (NOACs) must only be given postoperatively. Dabigatran is administered 4 hours and rivaroxaban 6 hours after surgery. In patients at high risk of bleeding or undergoing spinal anaesthesia anticoagulation should only be initiated a minimum of 12 hours postoperatively. Aspirin offers only weak VTE prophylaxis.97
Recommendation: There is no data specific to hernia repair. General surgical principles of DVT prophylaxis should be followed (Grade: Moderate).
Anaesthetic technique
General anaesthesia is most often used, but in certain situations, regional or local anaesthesia can be used depending on the size and location of the hernia.99,100
SECTION E: USE OF MESH
Wound healing is complex and is influenced by patient genetics (ratios of collagen and fibroblast subtypes), patient comorbidities affecting fibroblast-migration, biomechanical factors such as movement of the abdominal wall and pressure dynamics. Anatomical factors such as blood supply, potential spaces and technical factors relating to the repair or closure also play a role. Mesh provides a scaffold to facilitate granulation, fibroblast deposition and reorganisation.
There are 7 categories of mesh subtype available commercially. (see Table 6)
Selection of the most cost-effective appropriate mesh is determined by the approach, the position of the mesh and the risks for surgical site occurrences. The surgeon needs to weigh up properties of different types of mesh. These have different advantages in terms of tissue ingrowth, encapsulation, shrinkage, pore size, anti-adhesive characteristics, risk of sepsis and explanation, in vivo disintegration, foreign body reaction, abdominal wall compliance, burst strength and cost. (see Table 7)
The objective should be to select a mesh which promotes healing and strengthens the repair, while reducing sepsis, thick plates of granulation and chronic pain. Current thinking is that neither tensile strength nor mesh-weight are important determinants for good outcome, rather than adequate pore size of between 1-4 mm, coupled with a mesh of adequate burst pressure offer the most critical balance between good tissue ingrowth and protection from central mesh failure.101
The problem of shrinkage
Shrinkage is a universal problem and should be an important factor in deciding on mesh positioning and overlap.
Every mesh has a different capacity for shrinkage and every mesh behaves differently in different patients after implantation. To compensate for shrinkage, it is recommended to calculate shrinkage of approximately one-third for every mesh. Consequently, a mesh of 10 cm diameter for example will reduce to 8 cm. It follows therefore that even for very limited misplacement of mesh during fixation, a 5 cm overlap may be insufficient for a large hernia or excessive for small hernias. A 1 cm hernia should have a mesh of 7 cm minimum diameter. A hernia larger than 10 cm probably requires a larger overlap.
It is important to note that mesh overlap should be calculated by the pre-closure size of the defect and not after the fascial approximation has been performed.
Recommendation: A minimum overlap of 5 cm before defect closure should be planned in all mesh repairs (Grade: Strong).
Mesh selection and options for different types of ventral hernia
The most cost effective product that is available should be used for the appropriate indication. Mesh choice should therefore be individualised based on the following factors:
• Position of the mesh
• Presence of infection or contamination
• Risk of infection
Open Ventral Hernia Repair Mesh Selection: Based on the Ventral Hernia Working Group Classification,11 the HIG proposes the following strategy for mesh selection in Open Extraperitoneal Surgery: see Table 8.
Intraperitoneal mesh placement: The HIG recommends the following mesh options in the setting of intraperitoneal mesh placement: see Table 9
According to Brahmbhatt et al. the Ventral Hernia Working Group (VHWG) 2010 classification has little predictive value in laparoscopic ventral hernia repair (LVHR) and further independent risk factors in LVHR have been identified.13 Alternative risk stratification systems have been proposed but not widely adopted.
Adhesions after ventral hernia repair are a common phenomenon. There is no technique and no device that completely prevents the formation of adhesions. The risk of adhesions is greatly reduced by remaining outside the peritoneal cavity, though it does not eradicate the risk completely. Approximately two-thirds of patients will develop adhesions after LVHR.88
Direct contact of visceral organs to polypropylene and polyester is followed by variable degrees of adhesions to the mesh, which in turn may lead to a higher risk of bowel resection in case of revision operations. There is a widely held view that this may also predispose to mesh erosion and fistula formation, but there is no evidence that coated meshes reduce the incidence of these adverse events which are rare.88
The risk of adhesion formation has largely been ameliorated by the introduction of coated meshes or meshes such as expanded polytetrafluoroethylene (ePTFE) and polyvinylidene fluoride (PVDF).102 Whilst there is no proven superiority of one device or barrier over the next, barriers with long-term absorption profiles, or with small impenetrable pore size cause encapsulation and prevent tissue ingrowth.12
The use of uncoated polypropylene meshes and polyester meshes are not recommended for laparoscopic intraperitoneal onlay mesh (IPOM). Composite meshes and PTFE meshes are generally recommended for intraperitoneal use. 88,103-106
In 2000, Chowbey et al. reported about 202 laparoscopic ventral hernia repairs with the use of pure polypropylene meshes. In his series, there were two postoperative hernia recurrences at a mean follow-up of 2.9 years. There were no postoperative sequelae related to bowel adhesions.107 It is reported that in some low/middle income countries up to two-thirds of laparoscopic ventral hernia repairs are performed with unprotected polypropylene mesh because of costs.
Halm et al. reported a series on subsequent laparotomy / laparoscopy after intraperitoneal placed polypropylene meshes. The perioperative course was complicated in 76% of procedures. Small bowel resections were necessary in 21% of the cases. In 26%, the patients developed a surgical site infection.88
Infection and Contamination: Carbonell, in 2013, reported the recurrence rate in clean contaminated and contaminated fields to be similarly high (7% SSI in clean-contaminated 19% in contaminated).108 Mesh was explanted for anastomotic leaks, stomal revision and for an enterocutaneous fistula but not for mesh related complications.13,108
Sartelli reported on the safe use of plain polypropylene mesh in the setting of bowel ischaemia and bowel necrosis. There are numerous papers in the related field of inguinal hernia surgery which support the safe use of polypropylene mesh in contaminated fields.109
Compelling contradictory evidence was published by Choi et al. concluding that mesh should be avoided in cases with any level of contamination due to increased risk of postoperative adverse events.110
In the case of inadvertent contamination due to enterotomy, the following options can be considered:
• Suture the intestine and return at a later stage to repair the hernia.
• Suture the intestine and continue with an IPOM repair of the hernia. This should only be considered with minimal contamination, taking patient co-morbidities into account, with high level of surgical expertise. The possibility of enterotomy and management options should be discussed with the patient when taking consent. Avoid plain mesh, biologic mesh and PTFE.
• Convert to open procedure, suture the enterotomy and proceed with retrorectus repair.
Recommendations:
• The most cost-effective product that is available should be used for the appropriate indication (Grade: Strong).
• Extraperitoneal repairs in VHWG class I and II should be performed with plain large pore polypropylene or polyester mesh (Grade: Strong).
• Intraperitoneal mesh repairs should be performed with a composite barrier mesh or strand coated anti-adhesion mesh (Grade: Moderate).
• In contaminated wounds care should be taken to avoid the possibility of mesh sepsis, mesh explantation and wound complications. Use of polypropylene mesh in grade 3A wounds carries a high risk for septic complications (Grade: Moderate). Biologics or delayed fully resorbable meshes may be considered an alternative (Grade: Weak).
• In VHWG class 3C wounds there remains debate over the role of biologics. Evidence suggests that biologics perform poorly under these circumstances and may not warrant the high cost (Grade: Moderate).
Role of biologic meshes
When biologic acellular dermal matrices became available for use in complex hernia repairs, there was an initial flurry of enthusiasm and excitement and adoption of this prohibitively expensive material for the most challenging and complex of cases.
Unfortunately, the enthusiasm was short-lived as it turns out that biologics do not perform as well as one might have hoped in several of the more challenging scenarios.111
Biologic mesh is an acellular collagen matrix which has been derived from either human/porcine/bovine origin. Its role is to act as a bio-scaffold or platform for tissue integration and collagen regeneration. This scaffold is intended to biodegrade over time. Not all biologic meshes are re-engineered in the same way and the outcomes, particularly between cross-linked and non-cross-linked matrices may be vastly different.
Theoretically, collagen ingrowth leads to neovascularization, there is then delivery of macrophages and antibiotics to resist sepsis. However, in reality, there may be macrophage activation, which leads to an increased cytokine expression, increased inflammatory response and foreign body reaction, particularly when cross-linked matrices are used. The resultant encapsulation and poor tissue integration may account for the high recurrence rate of approximately 30%, a high failure rate and a very high degradation rate in the setting of sepsis.112,113
Itani et al. reported in the Repair of Infected or Contaminated Incisional Hernias (RICH) study a 28% recurrence at 2 years in a prospective observational cohort study of Strattice.114 This finding is notable because the median BMI was 30.9 kg/m2, 51% had prior mesh repair, and 51% had signs of infection prior to surgical repair, which is comparable with outcomes of synthetic mesh in non-contaminated fields.115 Rosen et al. also reported on a 5-year clinical experience in infected and contaminated hernias with biologic repair in 128 patients.116 The recurrence rate was approximately 20-23%, again comparable with some published data on synthetic mesh outcomes.
A highly cited review on the role of biologics in the contaminated field was published by Shankaran.103 The data included in this review was all retrospective in nature and heterogeneous, and some authors feel that the conclusions of this author are unsafe (IEHS).46,47 A further systematic review by Bellows states that there is a paucity of high quality data on the issue of biologics in contaminated fields.117 Interestingly, the use of biologic meshes in contaminated fields does not carry FDA clearance due to the disproportionately high number of adverse events.46,47,103,117
A recent meta-analysis by Huerta reported recurrence rates ranging from 0% to 80% and other inconsistencies in reported outcomes. They note that all biological mesh devices have been approved by the FDA based on substantive equivalence to a group of non-biological devices that, on average, were one-third less costly.118 They conclude that there is as yet no evidence to justify the cost of biologics in terms of outcome. In contrast, DeNoto states that the cost of the mesh is offset by the reduction in post-operative costs.119
The LAPSIS study looking at non-crosslinked biologic mesh in a bridging technique such as used for LVHR was prematurely terminated due to the poor outcomes - 19% recurrence vs 5% for synthetic mesh.120 Likewise, in a contaminated setting, bridging of defects with biological meshes should be avoided.121
A retrospective study looking at crosslinked biologic for bridging concluded that it was a safe alternative to composite meshes made of polypropylene and ePTFE for elective laparoscopic repair of incisional and ventral hernias.122
Recommendation: There is no evidence to support the routine use of biologic meshes. There may be a place for it in grade 3A and 3B wounds. (Grade: Moderate). The indications and clinical outcomes after use of biologics should be entered into registries or audited (Grade: Weak).
Is there a place for open suture repair?
Over the past 20 years there has been accruing evidence that the best outcomes for hernia repair are achieved with mesh reinforcement. Evolving evidence for the routine use of mesh continues to expand the pool of indications for its use. Despite many challenges, such as those offered by Burger in 2004, that "suture repair should be abandoned" many surgeons continue to perform at least some tissue repairs.123 Reasons why some surgeons not have adopted routine mesh placement may include concerns about increased complexity and cost of the procedure, or fear of complications.
Evidence: (see Table 10)
Large ventral hernias: Schumacher et al. reported in a retrospective analysis of recurrence rate after mesh-free Spitzy's repair a clear correlation between hernia size and BMI > 30 kg/m2 and the recurrence rate. The paper also illustrates the dramatic rise in recurrence rates with the size of the defect from 6.3% for defects under 1 cm to 54.5% for defects over 4 cm.124
Small Secondary Hernias: The 2008 Cochrane Analysis on 1141 patients shows a concordance of all RCTs in all but 2 cohort studies, that confirms that mesh repair decreases recurrence but increases SSI.125
Small Primary Hernias: In two very large prospective databases, it has been shown that mesh repair halves long-term risk of recurrence, and slightly increases readmission rates. There is no difference in chronic pain.42,126
Meta-analysis confirms that mesh repair has a small reduction in recurrence rate compared with suture repairs for primary ventral hernias, but an increased risk of seroma was observed.127,128 RCTs report a recurrence in umbilical hernia repair of 11% for suture vs. 1% for mesh.129 The risk or recurrence after suture repair increases to 19% after emergency repair.128
The only significant dissenting paper is a retrospective review of 306 umbilical hernia patients over 10 years. Complications were noted to be 6 times more common (OR 6.63; CI 95%) in mesh repairs with no risk reduction in recurrence (9% vs 8%).130
Recommendations:
• Every incisional hernia requires a mesh repair because there is a significantly lower recurrence rate (Grade: Strong).
• Primary ventral hernias with a defect greater than 2 cm require a mesh repair (Grade: Strong).
• Primary hernias less than 2 cm in patients with risk factors for recurrence (obesity, concurrent hernia, recurrent hernia, concurrent diastasis or aneurysmal disease) require a mesh repair (Grade: Strong).
• Mesh placement for small hernias less than 2 cm is the treatment of choice based on recurrence (Grade: Strong). These hernias can be repaired with suture alone with an acceptable recurrence rate of about 5% (Grade: Weak).
SECTION F: TECHNIQUE
Laparoscopic vs open ventral hernia repair
In the USA, approximately 56 000 isolated ventral hernia repairs are performed per year. In 2009 and 2010, 26.6% of these were performed laparoscopically and the remainder open.136 Comparative figures for South Africa are not available.
Limited data is available from multicentre trials looking at "real world" surgery.137 The Dutch incisional hernia (INCH) multicentre trial will start reporting results shortly; although only 130 patients in each arm are planned, this may shed some more light.138
High grade evidence comparing the two techniques is still dependent on relatively small numbers. The most recent meta-analysis includes only 1003 patients,139 and for incisional hernia specifically this is even smaller - 611140 or 751.141 Although all ventral hernias are commonly pooled in RCTs, it must be noted that there is a vast difference between primary ventral hernias and incisional hernias as far as difficulty, complications and recurrences are concerned.142,143
The following conclusions can be made from this available evidence:
• Laparoscopic repair results in significantly less surgical site infection for all ventral hernias.139,144,145 The rate of infection requiring mesh removal is not statistically significantly different for open and laparoscopic groups.146
• Laparoscopic repair results in more serious complications than open.147 These complications are more common in incisional hernias compared to primary hernias.148 The odds ratio for increased bowel injury in laparoscopic ventral hernia repair is reported to be 2.56141 to 3.68.139
• There is no significant difference in operating time between open and laparoscopic repair for all ventral hernias.139,144 When incisional hernia repair alone is analysed, there is borderline statistical significance which amounts to about 15 minutes longer theatre time in the laparoscopic group.140
• Laparoscopic repair may decrease length of hospitalization, but only in RCTs where LOS in the open group is inordinately long.144 There is no significant difference in the incisional hernia repair group.140,141
• There is no difference in short-term or long-term pain, patient satisfaction, reoperation rate, seroma rate, time back to work or body image between the two techniques.139-141,144,149
• There is no difference in short term recurrence rate. The follow-up in the most recent meta-analysis ranges from 2-35 months for incisional as well as pooled ventral hernias.139,140
• Laparoscopic repair has higher operative cost compared to open repair. One can argue that shorter hospital stays and quicker return to work, as well as less cost associated with SSI, leads to a cost advantage to society. This has not been shown in any prospective trial. Retrospective reviews showing reduced cost, do not take differences in size or complexity of hernias or patient status into account.150 These should not be used as a basis for decision making. There are no cost studies in South Africa and limited international studies from which to draw conclusions.151,152
• In meta-analyses there is no significant difference in quality of life after 6 months between open and laparoscopic repair.144,153 In choosing a technique, the surgeon should consider that bulging and poor cosmetic outcome were deemed more negative by patients than actual hernia recurrence.154
Recommendation: Open ventral hernia repair remains the standard, though the laparoscopic approach is a good alternative. The decision on approach should be based on patient wishes and surgical expertise as well as technical, anatomical and physiological factors (Grade: Moderate).
Technique: Laparoscopic ventral hernia repair.
Surgical principles in laparoscopic ventral and incisional hernia repair:
• Safe entry into the peritoneal cavity.
• Insufflation.
• Very careful adhesiolysis and reduction of the hernia contents.
• Clearing away the edges of the defect and wide mesh coverage of the defect.
• Fixing the mesh either to the posterior abdominal wall or trans-fascial fixation.
• Closure of the defect and/or component separation may be performed.
Further detailed discussion on surgical technique can be found in the comprehensive European and American guidelines.46,47,155
Should the primary defect be closed in laparoscopic repair?
Nguyen et al. reviewed available evidence and found no high quality evidence. Their systematic review of 11 studies included 8 case series and 3 comparative studies. These studies suggested that primary fascial closure (n = 138) compared to non-closure (n = 255) resulted in lower recurrence rates (0-5.7% vs. 4.8-16.7%) and seroma formation rates (5.6-11.4% vs. 4.3-27.8%). The maximum suggested size amenable to closure is 6-10 cm.156
Theoretical advantages to re-approximating the abdominal fascia of the hernia defect prior to mesh placement include:157,158
• Restoration of the abdominal muscles to a physiological position, possibly aiding in improved abdominal wall function.159
• The mesh is in contact with a greater surface area of abdominal wall (overlap for incorporation).
• There may be a decreased recurrence rate.160
• Reduced bulging of the mesh into the hernia.
• Bulging causes poor cosmetic results, and may allow mesh to come into contact with the skin, which can increase the risk of mesh erosion and subsequent infection.
Theoretical disadvantages of closing the defect:
• Approximating the edges of the defect increases tension, especially with larger defects, which may be counterproductive. Although this is counter intuitive for a so-called "tension-free" repair, current thinking supports repair under "physiological tension." 159,161
• Placement of extra sutures in the abdominal wall may increase the risk of postoperative pain. In large series, long-term pain after facial closure is comparable to other series without closure.154,160-162 In the series of Palanivelu, this amounted to 5% long term pain,160 and 2.56% in a large series of > 1 200 patients.161
• Longer operating time.
Size plays a substantial role in the decision about closure during laparoscopic repair. For small defects, particularly Swiss-cheese type defects, fascial closure may not be warranted unless a single defect is large (more than 2 cm wide). Closure of defects more than 6-10 cm can be challenging.
There is limited comparative literature but primary fascial closure may result in lower rates of eventration (bulging), recurrence and seroma formation. Patients appear to be more satisfied with the results and have improved functional status compared to a bridged repair.
Recommendation: Primary fascial closure of all defects greater than 2 cm in diameter is recommended (Grade: Moderate).
Fixation of mesh in laparoscopic repair
Two types of fixation methods are available: tacks and trans-fascial sutures. Both are available as absorbable or permanent types. There are developments utilising fibrin-based glue for fixation but the available evidence is limited. It is likely to play a bigger role in future after prospective evaluation.157
Proposed advantages of tacks only are shorter operative time, fewer skin incisions, improved cosmetic result and less acute and chronic pain. Advantages of suture only, are lower cost and stronger, more durable attachment of mesh.46,47,157,163
Nguyen et al. prospectively evaluated pain outcome and concluded that the choice of fixation method does not alter risk of postoperative pain.164
Colak et al. randomised fixation of mesh between absorbable and non-absorbable tackers. At mean follow-up of 31 months, there was no difference between pain and recurrence.163
In a recent large meta-analysis, Sajid et al. compared tacker mesh fixation with suture mesh fixation evaluating operative time, postoperative pain and complications including recurrence. Tackers were reported to decrease operative time, while the other parameters were comparable.165
Recommendation: Mesh should always be fixed using tackers (absorbable or non-absorbable), trans-fascial sutures or a combination (Grade: Strong). If a tacker alone is used, the defect should be closed (Grade: Weak).
Which mesh position is best in open hernia repair?
In laparoscopic ventral hernia repair, the mesh is routinely placed in the intra-peritoneal position. However, for open surgery, there are numerous options for mesh placement (Figure 2). Only (Overlay) repair places the mesh on the anterior fascia, which typically involves dissection of flaps and primary closure of the fascia below the mesh. Inlay repair places the mesh in the hernia defect and secures the mesh circumferentially to the edges of the fascia. Sublay repair refers to retrorectus or preperitoneal mesh placement. It is also commonly referred to as a Rives-Stoppa or retro-muscular repair. Finally, underlay repair is when mesh is placed in the intra-peritoneal position and secured to the anterior abdominal wall.166 The underlay is also referred to as an open intra-peritoneal onlay mesh (IPOM).
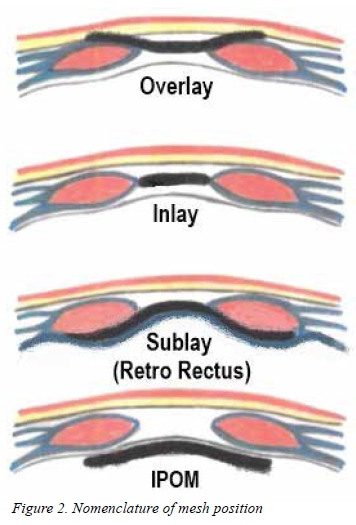
In the laparoscopic literature an IPOM refers to an intra-peritoneal mesh position which is equivalent to an underlay mesh position.
Holihan performed an exhaustive meta-analysis of 21 available trials with almost 6 000 patients comparing the above different mesh positions.166
Retrorectus: On multiple treatment analysis, retrorectus was ranked as the best mesh placement option with a high probability of being the best treatment. Retrorectus repair had a 94.2% probability of having the lowest odds for recurrence and a 77.3% probability of having the lowest odds for SSI.
Open IPOM: While underlay (IPOM) had the second highest probability of being the best treatment, it remained a distant second. The probability of it having the lowest odds of recurrence was only 5.8% and for SSI was 11.4%.
Onlay: On multiple-treatment meta-analysis, onlay was one of the worst mesh placement options with a very low probability (0.001) of being the best treatment.
Inlay: Inlay was associated with higher odds for recurrence and SSI than onlay, retrorectus and underlay. Inlay was one of the worst mesh placement options with a very low probability (0.001) of being the best treatment.
In addition, the authors comment that the retrorectus technique, although perceived to be technically challenging, is easily and reproducibly learnt. No evidence is available on the learning curve. Notwithstanding whether the retrorectus or underlay technique is used, the authors recommend an overlap of at least 3-5 cm.
Breuing et al. reviewed the literature for the Ventral Hernia Working Group. Their treatment algorithm suggests primary closure with mesh reinforcement for small hernias, and component separation to restore the midline muscles together with mesh reinforcement for all other hernias. The authors suggest a minimum overlap of 5 cm.11
Albino et al. did a systematic review of the literature on mesh placement. They identified 62 studies with 5 824 patients. The recurrence rate and postoperative infection rate of retrorectus and underlay techniques were the lowest, with a trend favouring retrorectus.167
Both Deerenberg and Eriksson did systematic reviews of the treatment of large and giant incisional hernia.168,169 Both groups of authors conclude that the retrorectus method, possibly combined with component separation, is the best technique for this challenging group. They also stress that large and giant incisional hernias offer specific technical challenges and should best be repaired by specialist hernia surgeons.
Recommendations: All open incisional hernias should be repaired using mesh (Grade: Strong). The mesh should be placed in a retrorectus position. If not possible, the mesh should be placed in an underlay position (IPOM). The use of onlay and inlay mesh is discouraged (Grade: Strong).
SECTION G: COMPLICATIONS
Most complications after ventral hernia surgery are minor and will resolve within 8 weeks. Major complications can have devastating consequences for the patient.
Laparoscopic repair has a lower total rate of complications at 8 weeks postoperatively when compared to open repair. When complications do occur these are more severe in the laparoscopic repair group.139,144
Intraoperative complications:
Enterotomy: Enterotomy occurs between 1-6% in the reported literature, usually during adhesiolysis.114,141 The risk for enterotomy is higher during laparoscopic repair.170 Adhesiolysis should be performed carefully with sharp and/or blunt dissection with minimal usage of energy devices for haemostasis and should include the full length of the old scar. Direct traction on the bowel should be avoided.
Careful inspection of the bowel after adhesiolysis is recommended. A recognised enterotomy should be repaired immediately to minimise contamination.102,146
The intestinal repair can be done laparoscopically with a simple suture repair or conversion to an open procedure. The decision should be based on the severity of the enterotomy, contamination and the surgeon's skill.48
Recommendation: Careful inspection of the bowel pre, intra and post dissection should be carried out to avoid missed enterotomy (Grade: Strong).
Post-Operative Complications
Unrecognized enterotomy: This is a devastating complication for patient and surgeon. Delayed presentation of enterotomy should be managed urgently at recognition. Repair is feasible laparoscopically but will usually require urgent laparotomy and bowel repair.170
Causes include: unrecognized intra-operative enterotomy, thermal injuries or enterotomy due to fixation devices when placing and fixing the mesh.157,171
Strongly consider removing mesh at the time of bowel repair based on the degree of soiling, the time passed since perforation, the type of mesh and the clinical condition of the patient. Options for closure of the abdominal wall include temporary closure, biological meshes, simple sutured repair, sandwich and vacuum techniques.172
Mechanical obstruction: The incidence after ventral hernia repair ranges from 0.5 to 1%. This is due to mesh slippage and bowel entrapment between mesh and abdominal wall, adhesions (mostly on the exposed tacks or borders of the mesh) or strangulation of bowel in a port site.
The diagnosis should be confirmed with X-rays or a CT scan. Most uncomplicated obstructions resolve with conservative management.139,173
Prolonged ileus: The possibility of an unrecognised enterotomy and mechanical obstruction must be excluded before making the diagnosis of ileus. Ileus after hernia repair is reported in up to 16% of cases. Conservative management is usually effective.48
Recommendations: a high index of suspicion should be maintained in every patient having undergone hernia repair given the potential for mortality and morbidity in the case of unrecognised enterotomy. (Grade: Strong)
Wound and mesh infection: The incidence of mesh infection in open and laparoscopic ventral hernia repair is low, reportedly less than 1%.146
Laparoscopic ventral hernia repair has a lower rate of wound infection compared to open repair.48,144
Large pore size (1-4 mm) is associated with less infection rates and increased mesh salvage rates in open repair.174,175
Mesh salvage may be successful by using antibiotics, percutaneous drainage, wound debridement and negative pressure dressings. When attempting to salvage the mesh, consider incorporation of the mesh, possible exposure of mesh, bowel integrity (exclude a fistula) and the patient's clinical condition175,176
Recommendation: Superficial wound sepsis should be managed with standard conservative means. Deep surgical site infection with the possibility of mesh sepsis may require explantation for resolution (Grade: Moderate).
Seroma and haematoma: Seromas are a common complication after ventral hernia repair. These are treated conservatively and usually resolve spontaneously. Persistent seromas are defined as seromas that persist for more than 8-12 weeks postoperatively.147 About one-third of persistent symptomatic seromas will require aspiration due to symptoms. Aspiration carries a risk of infection and should be done with strict sterile technique.177 Conservative management of seromas does not have an increased risk for infection.154 Failed aspiration of seromas can also be addressed by excision.157
Techniques to minimize seroma formation have mixed outcomes and no one technique has been proven to be effective.147,177,178
Recommendation: Conservative management of seroma is largely successful (Grade: Moderate).
Postoperative bulging: Exclusion of hernia recurrence is important. This can be done clinically, but may require a CT scan. Patients often have a negative perception about a postoperative bulge.85 This negatively influences their quality of life and should be prevented. Sheath defect closure helps to restore the abdominal wall contouring and thus bulging in the area of the hernia defect.149 Standard physiotherapy and biokinetic rehabilitation may be beneficial. The decision to re-operate should be made by the combined treating team. Patients can be reassured if asymptomatic.
Post-operative pain: Postoperative pain rates are similar between open and laparoscopic ventral hernia repair and should have resolved by 6 weeks.114,179
Persistent pain is defined as pain that persists longer than 6-8 weeks. Causes for persistent pain may be seroma or haematoma formation, sutures or tacks, adhesions, bowel entrapment, mesh infection and shrinkage. This may need to be evaluated by CT scan.108,160,180
Persistent pain should be managed with: analgesics, anti-inflammatory medication, steroids and nerve blocks in the absence of a definite cause seen on CT scan.144,160,180,181
Persistent pain after the above-mentioned measures can be managed by removal of tacks or trans-fascial sutures in the area of pain, and in some cases, necessitates removal of the mesh.144,160,180,181
Recommendation: Persistent pain is a severe adverse outcome and should be investigated and managed (Grade: Strong).
Recurrence: Recurrence rates are similar between open and laparoscopic approaches.178 Symptomatic recurrence should be surgically addressed when indicated according to the general principles discussed in earlier chapters.
SECTION H: SPECIAL TECHNIQUES
Is laparoscopic pre-peritoneal ventral hernia repair feasible?
These repairs are possible by adapting the TAPP and TEP techniques to repair small and medium-sized primary and incisional hernias of the abdominal wall.
Epigastric, suprapubic, umbilical, port site, Spigelian and lateral abdominal wall hernias can be repaired using a TAPP or a TEP approach. A single port technique has also been described.182-186
In the literature mainly case reports and the odd prospective cohort trial are available.
From these reports all the advantages of TAPP and TEP are evident:
• Removal of the hernia sac.
• Standard meshes are used.
• Closure of the defect and adequate mesh overlap is possible.
• Minimal fixation is required.
• Complication rates are low.
These procedures can be technically demanding and operating times may be longer than for open procedures.
Recommendation: Although these approaches are feasible, they are technically challenging, the outcomes and benefits are unclear and they should be performed by experienced hernia surgeons in a setting of ongoing audit only (Grade: Weak).
The role of endoscopic component separation (ECS)
Open component separation (OCS) was described by Ramirez et al. in 1990.187 OCS gives an abdominal wall release of at least 10 cm on each side, but involves extensive dissection of the subcutaneous tissue, thereby interrupting the blood supply to the skin and subcutaneous tissue. This results in a high incidence of skin necrosis and wound infection.
Rosen et al. described an endoscopic component separation technique (ECS) using a balloon dilator.188 ECS can be combined with laparoscopic or open hernia repair, with or without mesh placement. The lateral abdominal wall release obtained with ECS is not as extensive as with OCS, but fewer major wound complications are reported (41% vs 19%).189 ECS can be very useful in a contaminated abdominal wall reconstruction.
Relative contra-indications for ECS are previous transverse abdominal wall incisions and previous OCS.
Recommendation: The advantages of endoscopic ECS have largely been surpassed by the uptake of posterior component separation performed concurrently with a retrorectus dissection (Grade: Weak).
Posterior component separation
If, in a retrorectus repair (RIVES- STOPPA), adequate mesh overlap is not possible, further lateral mobilization can be done in either the preperitoneal space, or in the intermuscular space between transversus and internal oblique muscles. The latter has the potential complication of neuro-vascular damage to the rectus muscle, and affords no medial fascial advancement as none of the abdominal muscles can be divided and released.190
The preperitoneal space between transversus abdominis and peritoneum/ transversalis fascia can be dissected all the way back to the psoas muscle. This space is entered after division of the transversus abdominis muscle just lateral to its insertion into the posterior rectus sheath. This dissection results in huge medial fascial advancement and a big retroperitoneal space for mesh placement.
This technique can be used in the place of a traditional anterior component separation, avoiding the creation of huge skin flaps with all the associated post-op wound complications. In exceptionally large hernias and/or loss of domain, posterior component separation can be combined with OCS or ECS.191,192
Recommendation: PCS is the component separation procedure of choice to obtain medial fascial advancement and the creation of a huge space for mesh placement (Grade: Moderate).
Parastomal hernia repair
The incidence of parasternal hernia formation is between 30-50%. Traditional open repair bears the risk of the development of incisional hernia formation and has a higher incidence of wound infections.
Technique of repair: Three laparoscopic operations have been described: the modified keyhole technique,193 the modified Sugarbaker194 technique and a combination of the two - the sandwich technique. The modifications of the first two techniques involve adequate mesh overlap of at least 5 cm.
The keyhole procedure involves a slit in the mesh for passage of the bowel loop. The reported recurrence rate for this procedure is between 37-73%.195 In the Sugarbaker operation the bowel loop passes laterally from under the mesh, and the mesh overlies the hernia defect and the bowel loop. The reported recurrence rate for the Sugarbaker operation is between 4-5%. Berger reported a 0% recurrence with the sandwich technique.196
Mesh without an anti-adhesive barrier has been implicated in bowel erosion, adhesions and intestinal obstruction and is best avoided.197 However, many of these complications may be due to the extensive adhesiolysis with unrecognised bowel injuries.
Emergency repair: Mortality and morbidity rates after emergency parastomal hernia repair are very high, in keeping with outcomes in other emergency hernia surgery. Mortality is recorded at 25% and re-operation rates at 34% in a recent analysis of the Danish Registry. Adverse events and death are 10-fold higher for emergency repair as compared to elective parastomal hernia repair.42
Prophylactic mesh: The emphasis in future should be on prevention of parastomal hernias for permanent stomas. Patients should be given the choice of having a mesh placed prophylactically at the time of stoma creation.
A recent Danish study reported an unacceptably high early morbidity and recurrence rate after elective parastomal hernia repair. Their reported 25% risk for 30-day mortality after an emergency parasternal repair confirms the importance of prevention of parasternal hernias by prophylactic mesh placement at the time of stoma creation.42
One prospective randomised trial compared 54 patients receiving either a standard colostomy without mesh or a sublay of UltraPro. After 5 years, hernias were seen in 13% in the mesh group vs. 81% in the conventional colostomy group.198 Morbidity was very low. Two further trials showed similar results, making prophylactic mesh placement a safe option.199,200
Recommendation: Patients presenting with a parastomal hernia should be advised to have an elective repair to avoid the complications accompanying emergency presentation (Grade: Strong). Patients having a permanent stoma fashioned should be offered prophylactic mesh placement (Grade: Strong).
Diastasis of the rectus abdominis
Rectus diastasis is defined as the widening of the inter-rectus fascial distance. It is not a true hernia and does not carry the risk of bowel strangulation. In men, it occurs mostly above the umbilicus and is associated with increased intra-abdominal fat. In women, it mostly follows multiple pregnancies, and is centred around the umbilicus, but can extend up towards the xiphisternum and down towards the symphysis pubis. Traditional reasons for repair have ranged from cosmetic reasons to debilitating weakness of the abdominal wall in multiparous women.
Surgical repair includes simple suture plication with or without abdominoplasty. Cosmetic surgeons often add an onlay mesh to reinforce the suture plication. Retrorectus mesh repair is reported to have a lower recurrence rate than onlay mesh repair. Reports of posterior component separation with mesh placement for large defects, as well as laparoscopic plications and IPOM mesh repair are reported in the literature.201,202
For a co-existing midline hernia associated with the diastasis a retrorectus mesh repair should be done to prevent recurrence. The reported complications are mostly minor seromas and superficial skin infections and skin necrosis. Recurrence after mesh repair is rare, but up to 40% of suture plications recur.201,202
Non-operative strategies such as physiotherapy and weight loss programmes remain the mainstay of therapy in patients without concurrent hernia.
Recommendation: Rectus diastasis accompanied by a midline hernia should be repaired with a retrorectus mesh (Grade: Strong). Rectus diastasis without concurrent hernia should not be repaired unless there is compelling evidence of loss of core muscle stability and function (Grade: Weak).
Conclusion
Ventral hernia surgery ranges in complexity from the simplest small primary midline defect, to complex redo surgery, in patients with significant anatomical challenges and co-morbidities. In order to obtain the best possible outcomes for the patient, it is necessary for the surgeon to possess a sound foundation in the principles of ventral hernia repair as well as a range of skills and options for managing these patients. The HIG believes that the best results will be achieved when surgeons commit themselves to continuous professional development and the auditing of outcomes in the format of a national registry.
The HIG also believes that the development of guidelines for hernia management in the South African environment is a critical step in achieving the goal of excellence in hernia care. We note that new data emerges on a continuous basis and the intention is to revise these guidelines on a 3 yearly cycle.
Conflict of Interest Statement
The Hernia Interest Group has a relationship with the following companies: Ascendis; Bard; Johnson and Johnson; KCI (Acelity); Medtronic and SABiomedical. This association extends to funding for congress participation and academic activities, facilitation of training and administrative costs. The industry in no way provided input for, or participated in the consensus meetings, or creation of these guidelines.
Acknowledgements
The HIG extends its gratitude to Mrs Susan Parkes whose administrative assistance was greatly valued. Individual members also acknowledge with gratitude, their families for the support extended during this authorship.
REFERENCES
1. Kingsnorth A, LeBlanc K. Hernias: Inguinal and incisional. The Lancet. 2003;362(9395):1561-1571. [ Links ]
2. Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am. 2003;83(5):1045-1051. [ Links ]
3. Alnassar S, Bawahab M, Abdoh A, Guzman R, Al Tuwaijiri T, Louridas G. Incisional hernia postrepair of abdominal aortic occlusive and aneurysmal disease: Five-year incidence. Vascular. 2012;20(5):273-277. [ Links ]
4. Helgstrand F, Rosenberg J, Bay-Nielsen M, et al. Establishment and initial experiences from the Danish ventral hernia database. Hernia. 2010;14(2):131-135. [ Links ]
5. Korenkov M, Paul A, Sauerland S, et al. Classification and surgical treatment of incisional hernia. Langenbeck's Arch Surg. 2001;386(1):65-73. [ Links ]
6. Indicators IQ. Agency for healthcare research and quality . 2002. [ Links ]
7. Muysoms F, Miserez M, Berrevoet F, et al. Classification of primary and incisional abdominal wall hernias. Hernia. 2009;13(4):407-414. [ Links ]
8. Singal R, Dalal U, Dalal AK, et al. Traumatic anterior abdominal wall hernia: A report of three rare cases. J Emerg Trauma Shock. 2011;4(1):142-145. [ Links ]
9. Earle DB, McLellan JA. Repair of umbilical and epigastric hernias. Surg Clin North Am. 2013;93(5):1057-1089. [ Links ]
10. Burcharth J, Pedersen M, Pommergaard H, Bisgaard T, Pedersen C, Rosenberg J. The prevalence of umbilical and epigastric hernia repair: A nationwide epidemiologic study. Hernia. 2015;19(5):815-819. [ Links ]
11. Breuing K, Butler CE, Ferzoco S, et al. Incisional ventral hernias: Review of the literature and recommendations regarding the grading and technique of repair. Surgery. 2010;148(3):544-558. [ Links ]
12. Berger RL, Li LT, Hicks SC, Davila JA, Kao LS, Liang MK. Development and validation of a risk-stratification score for surgical site occurrence and surgical site infection after open ventral hernia repair. J Am Coll Surg. 2013;217(6):974-982. [ Links ]
13. Brahmbhatt R, Carter SA, Hicks SC, Berger DH, Liang MK. Identifying risk factors for surgical site complications after laparoscopic ventral hernia repair: Evaluation of the ventral hernia working group grading system. Surgical infections. 2014;15(3):187-193. [ Links ]
14. Oodit R. Hernia surgery, South Africa 2015 : Editorial. South African Journal of Surgery. 2015;53(2):37. [ Links ]
15. Burger JW, Lange JF, Halm JA, Kleinrensink G, Jeekel H. Incisional hernia: Early complication of abdominal surgery. World J Surg. 2005;29(12):1608-1613. [ Links ]
16. Muysoms F, Antoniou S, Bury K, et al. European hernia society guidelines on the closure of abdominal wall incisions. Hernia. 2015;19(1):1-24. [ Links ]
17. Franchi M, Ghezzi F, Buttarelli M, Tateo S, Balestreri D, Bolis P. Incisional hernia in gynecologic oncology patients: A 10-year study. Obstetrics & Gynecology. 2001;97(5):696-700. [ Links ]
18. Beadles CA, Meagher AD, Charles AG. Trends in emergent hernia repair in the United States. JAMA Surgery. 2015;150(3):194-200. [ Links ]
19. Derici H, Unalp H, Bozdag A, Nazli O, Tansug T, Kamer E. Factors affecting morbidity and mortality in incarcerated abdominal wall hernias. Hernia. 2007;11(4):341-346. [ Links ]
20. Le Huu Nho R, Mege D, Ouaissi M, Sielezneff I, Sastre B. Incidence and prevention of ventral incisional hernia. J Visc Surg. 2012;149(5 Suppl):e3-14. [ Links ]
21. Shell DH, De La Torre J, Andrades P, Vasconez LO. Open repair of ventral incisional hernias. Surg Clin North Am. 2008;88(1):61-83. [ Links ]
22. Bucknall TE, Cox PJ, Ellis H. Burst abdomen and incisional hernia: A prospective study of 1129 major laparotomies. Br Med J (Clin Res Ed). 1982;284(6320):931-933. [ Links ]
23. Israelsson LA, Jonsson T. Overweight and healing of midline incisions: The importance of suture technique. Eur J Surg. 1997;163(3):175-180. [ Links ]
24. Bevis P, Windhaber R, Lear P, Poskitt K, Earnshaw J, Mitchell D. Randomized clinical trial of mesh versus sutured wound closure after open abdominal aortic aneurysm surgery. Br J Surg. 2010;97(10):1497-1502. [ Links ]
25. Lamont P, Ellis H. Incisional hernia in re-opened abdominal incisions: An overlooked risk factor. Br J Surg. 1988;75(4):374-376. [ Links ]
26. Hoer J, Lawong G, Klinge U, Schumpelick V. Factors influencing the development of incisional hernia. A retrospective study of 2,983 laparotomy patients over a period of 10 years. Chirurg. 2002;73(5):474-480. [ Links ]
27. Serensen LT, Hemmingsen UB, Kirkeby LT, Kallehave F, Jergensen LN. Smoking is a risk factor for incisional hernia. Arch Surg. 2005;140(2):119-123. [ Links ]
28. Jenkins T. The burst abdominal wound: A mechanical approach. Br J Surg. 1976;63(11):873-876. [ Links ]
29. Moussavian MR, Schuld J, Dauer D, et al. Long term follow up for incisional hernia after severe secondary peritonitis-incidence and risk factors. Am J Surg. 2010;200(2):229-234. [ Links ]
30. Cheesborough JE, Dumanian GA. Simultaneous prosthetic mesh abdominal wall reconstruction with abdominoplasty for ventral hernia and severe rectus diastasis repairs. Plast Reconstr Surg. 2015;135(1):268-276. [ Links ]
31. Köhler G, Luketina R, Emmanuel K. Sutured repair of primary small umbilical and epigastric hernias: Concomitant rectus diastasis is a significant risk factor for recurrence. World J Surg. 2015;39(1):121-126. [ Links ]
32. Cox PJ, Ausobsky JR, Ellis H, Pollock AV. Towards no incisional hernias: Lateral paramedian versus midline incisions. J R Soc Med. 1986;79(12):711-712. [ Links ]
33. Brown SR, Tiernan J. Transverse verses midline incisions for abdominal surgery. The Cochrane Library. 2005. [ Links ]
34. Singh R, Omiccioli A, Hegge S, McKinley C. Does the extraction-site location in laparoscopic colorectal surgery have an impact on incisional hernia rates? Surg Endosc. 2008;22(12):2596-2600. [ Links ]
35. Copeland GP. The POSSUM system of surgical audit. Arch Surg. 2002;137(1):15-19. [ Links ]
36. Israelsson LA, Millbourn D. Prevention of incisional hernias: How to close a midline incision. Surg Clin North Am. 2013;93(5):1027-1040. [ Links ]
37. Deerenberg EB, Harlaar JJ, Steyerberg EW, et al. Small bites versus large bites for closure of abdominal midline incisions (STITCH): A double-blind, multicentre, randomised controlled trial. The Lancet. 2015;386(10000):1254-1260. [ Links ]
38. Petter-Puchner A. The state of midline closure of the abdominal wall. Br J Surg. 2015;102(12):1446-1447. [ Links ]
39. Diener MK, Voss S, Jensen K, Buchler MW, Seiler CM. Elective midline laparotomy closure: The INLINE systematic review and meta-analysis. Ann Surg. 2010;251(5):843-856. [ Links ]
40. Van't Riet M, Steyerberg E, Nellensteyn J, Bonjer H, Jeekel J. Meta-analysis of techniques for closure of midline abdominal incisions. Br J Surg. 2002;89(11):1350-1356. [ Links ]
41. Helgstrand F, Rosenberg J, Kehlet H, Jorgensen LN, Wara P, Bisgaard T. Risk of morbidity, mortality, and recurrence after parastomal hernia repair: A nationwide study. Dis Colon Rectum. 2013;56(11):1265-1272. [ Links ]
42. Helgstrand F. National results after ventral hernia repair. Dan Med J. 2016;63(7):B5258. [ Links ]
43. Swank H, Mulder I, La Chapelle C, Reitsma J, Lange J, Bemelman W. Systematic review of trocar-site hernia. Br J Surg. 2012;99(3):315-323. [ Links ]
44. Tonouchi H, Ohmori Y, Kobayashi M, Kusunoki M. Trocar site hernia. Arch Surg. 2004;139(11):1248-1256. [ Links ]
45. Armananzas L, Ruiz-Tovar J, Arroyo A, et al. Prophylactic mesh vs suture in the closure of the umbilical trocar site after laparoscopic cholecystectomy in high-risk patients for incisional hernia. A randomized clinical trial. J Am Coll Surg. 2014;218(5):960-968. [ Links ]
46. Bittner R, Bingener-Casey J, Dietz U, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (international endohernia society (IEHS)-part 1. Surg Endosc. 2014;28(1):2-29. [ Links ]
47. Bittner R, Bingener-Casey J, Dietz U, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (international endohernia society [IEHS])-part 2. Surg Endosc. 2014;28(2):353-379. [ Links ]
48. Cuccurullo D, Piccoli M, Agresta F, et al. Laparoscopic ventral incisional hernia repair: Evidence-based guidelines of the first Italian consensus conference. Hernia. 2013;17(5):557-566. [ Links ]
49. Lauscher JC, Martus P, Stroux A, et al. Development of a clinical trial to determine whether watchful waiting is an acceptable alternative to surgical repair for patients with oligosymptomatic incisional hernia: Study protocol for a randomized controlled trial. Trials. 2012;13(1):1. [ Links ]
50. Hjaltason E. Incarcerated hernia. Acta Chir Scand. 1981;147(4):263-267. [ Links ]
51. Davies M, Chris D, Gareth M, Ken S. Emergency presentation of abdominal hernias: Outcome and reasons for delay in treatment-a prospective study. The Annals of The Royal College of Surgeons of England. 2007;89(1):47-50. [ Links ]
52. Nieuwenhuizen J, Halm J, Jeekel J, Lange J. Natural course of incisional hernia and indications for repair. Scandinavian Journal of Surgery. 2007;96(4):293-296. [ Links ]
53. Vardanian AJ, Farmer DG, Ghobrial RM, Busuttil RW, Hiatt JR. Incisional hernia after liver transplantation. J Am Coll Surg. 2006;203(4):421-425. [ Links ]
54. Alani A, Page B, O'Dwyer P. Prospective study on the presentation and outcome of patients with an acute hernia. Hernia. 2006;10(1):62-65. [ Links ]
55. Read RC, Yoder G. Recent trends in the management of incisional herniation. Arch Surg. 1989;124(4):485-488. [ Links ]
56. Flum DR, Horvath K, Koepsell T. Have outcomes of incisional hernia repair improved with time?: A population-based analysis. Ann Surg. 2003;237(1):129-135. [ Links ]
57. Nieuwenhuizen J, Kleinrensink GJ, Hop W, Jeekel J, Lange J. Indications for incisional hernia repair: An international questionnaire among hernia surgeons. Hernia. 2008;12(3):223-225. [ Links ]
58. Kingsnorth AN. Hunterian lecture. Hernia surgery: From guidelines to clinical practice. Ann R Coll Surg Engl. 2009;91(4):273-279. [ Links ]
59. Birkmeyer J, Finlayson E. Volume and outcome-reply. N Engl J Med. 2002;347(9):695-695. [ Links ]
60. Neumayer LA, Gawande AA, Wang J, et al. Proficiency of surgeons in inguinal hernia repair: Effect of experience and age. Ann Surg. 2005;242(3):344-352. [ Links ]
61. Aikoye A, Harilingam M, Khushal A. The impact of high surgical volume on outcomes from laparoscopic (totally extra peritoneal) inguinal hernia repair. Journal of Clinical and Diagnostic Research: JCDR. 2015;9(6):PC15. [ Links ]
62. Kockerling F, Berger D, Jost JO. What is a certified hernia center? The example of the German Hernia Society and German Society of General and Visceral Surgery. Front Surg. 2014;1:26. [ Links ]
63. Birgisson G, Park A, Mastrangelo M, Witzke D, Chu U. Obesity and laparoscopic repair of ventral hernias. Surg Endosc. 2001;15(12):1419-1422. [ Links ]
64. Tsereteli Z, Pryor B, Heniford B, Park A, Voeller G, Ramshaw B. Laparoscopic ventral hernia repair (LVHR) in morbidly obese patients. Hernia. 2008;12(3):233-238. [ Links ]
65. Regner JL, Mrdutt MM, Munoz-Maldonado Y. Tailoring surgical approach for elective ventral hernia repair based on obesity and national surgical quality improvement program outcomes. Am J Surg. 2015;210(6):1024-1030. [ Links ]
66. Novitsky YW, Cobb WS, Kercher KW, Matthews BD, Sing RF, Heniford BT. Laparoscopic ventral hernia repair in obese patients: A new standard of care. Arch Surg. 2006;141(1):57-61. [ Links ]
67. Raftopoulos I, Courcoulas A. Outcome of laparoscopic ventral hernia repair in morbidly obese patients with a body mass index exceeding 35 kg/m2. Surg Endosc. 2007;21(12):2293-2297. [ Links ]
68. Froylich D, Segal M, Weinstein A, Hatib K, Shiloni E, Hazzan D. Laparoscopic versus open ventral hernia repair in obese patients: A long-term follow-up. Surg Endosc. 2016;30(2):670-675. [ Links ]
69. Lee DY, Rehmani SS, Guend H, et al. The incidence of trocar-site hernia in minimally invasive bariatric surgery: A comparison of multi versus single-port laparoscopy. Surg Endosc. 2013;27(4):1287-1291. [ Links ]
70. Marx L, Raharimanantsoa M, Mandala S, D'Urso A, Vix M, Mutter D. Laparoscopic treatment of incisional and primary ventral hernia in morbidly obese patients with a BMI over 35.Surg Endosc. 2014;28(12):3310-3314. [ Links ]
71. Ching SS, Sarela AI, Dexter SP, Hayden JD, McMahon MJ. Comparison of early outcomes for laparoscopic ventral hernia repair between nonobese and morbidly obese patient populations. Surg Endosc. 2008;22(10):2244-2250. [ Links ]
72. Kaoutzanis C, Leichtle S, Mouawad N, et al. Risk factors for postoperative wound infections and prolonged hospitalization after ventral/incisional hernia repair. Hernia. 2015;19(1):113-123. [ Links ]
73. Kamer E, Unalp HR, Derici H, Tansug T, Onal MA. Laparoscopic cholecystectomy accompanied by simultaneous umbilical hernia repair: A retrospective study. J Postgrad Med. 2007;53(3):176-180. [ Links ]
74. Praveen Raj P, Ganesh MK, Senthilnathan P, Parthasarathi R, Rajapandian S, Palanivelu C. Concomitant laparoscopic intraperitoneal onlay mesh repair with other clean contaminated procedures-study of feasibility and safety. J Laparoendosc Adv Surg Tech. 2015;25(1):33-36. [ Links ]
75. Ergul Z, Ersoy E, Kulacoglu H, Olcucuoglu E, Devay AO, Gundogdu H. A simple modified technique for repair of umbilical hernia in patients undergo laparoscopic cholecystectomy. report of 10 cases. G Chir. 2009;30(10):437-439. [ Links ]
76. Raziel A, Sakran N, Szold A, et al. Mid-term follow-up after laparoscopic sleeve gastrectomy in obese adolescents. Isr Med Assoc J. 2014;16(1):37-41. [ Links ]
77. Patel PV, Merchant AM. Ventral hernia repair in the morbidly obese patient: A review of medical and surgical approaches in the literature. Bariatr Surg Pract Patient Care. 2014;9(2):61-65. [ Links ]
78. Coelho JC, Claus CM, Campos AC, Costa MA, Blum C. Umbilical hernia in patients with liver cirrhosis: A surgical challenge. World J Gastrointest Surg. 2016;8(7):476-482. [ Links ]
79. Gray SH, Vick CC, Graham LA, Finan KR, Neumayer LA, Hawn MT. Umbilical herniorrhapy in cirrhosis: Improved outcomes with elective repair. J Gastrointest Surg. 2008;12(4):675-681. [ Links ]
80. Marsman HA, Heisterkamp J, Halm JA, Tilanus HW, Metselaar HJ, Kazemier G. Management in patients with liver cirrhosis and an umbilical hernia. Surgery. 2007;142(3):372-375. [ Links ]
81. Eker HH, van Ramshorst GH, de Goede B, et al. A prospective study on elective umbilical hernia repair in patients with liver cirrhosis and ascites. Surgery. 2011;150(3):542-546. [ Links ]
82. Kwon HJ, Chun JM, Kim SG, Kim HK, Huh S, Hwang YJ. Deceased donor liver transplantation performed one week after small bowel resection for complicated umbilical hernia: A case report. Korean J Hepatobiliary Pancreat Surg. 2014;18(3):94-96. [ Links ]
83. McKay A, Dixon E, Bathe O, Sutherland F. Umbilical hernia repair in the presence of cirrhosis and ascites: Results of a survey and review of the literature. Hernia. 2009;13(5):461-468. [ Links ]
84. Ammar SA. Management of complicated umbilical hernias in cirrhotic patients using permanent mesh: Randomized clinical trial. Hernia. 2010;14(1):35-38. [ Links ]
85. Schoenmaeckers EJ, Wassenaar EB, Raymakers J, Rakic S. Bulging of mesh after laparoscopic repair of ventral and incisional hernias. JSLS. 2010;14(4):541. [ Links ]
86. Ghnnam WM, Helal AS, Fawzy M, Ragab A, Shalaby H, Elrefaay E. Paraumbilical hernia repair during cesarean delivery. Ann Saudi Med. 2009;29(2):115-118. [ Links ]
87. Jensen K, Henriksen N, Jorgensen L. Abdominal wall hernia and pregnancy: A systematic review. Hernia. 2015;19(5):689- 696. [ Links ]
88. Halm J, De Wall L, Steyerberg E, Jeekel J, Lange J. Intraperitoneal polypropylene mesh hernia repair complicates subsequent abdominal surgery. World J Surg. 2007;31(2):423-429. [ Links ]
89. Ross SW, Wormer BA, Kim M, et al. Defining surgical outcomes and quality of life in massive ventral hernia repair: An international multicenter prospective study. Am J Surg. 2015;210(5):801-813. [ Links ]
90. Martindale RG, Deveney CW. Preoperative risk reduction: Strategies to optimize outcomes. Surg Clin North Am. 2013;93(5):1041-1055. [ Links ]
91. Latham R, Lancaster AD, Covington JF, Pirolo JS, Thomas CS. The association of diabetes and glucose control with surgical-site infections among cardiothoracic surgery patients. Infect Control Hosp Epidemiol. 2001;22(10):607-612. [ Links ]
92. Krpata DM, Criss CN, Gao Y, et al. Effects of weight reduction surgery on the abdominal wall fascial wound healing process. J Surg Res. 2013;184(1):78-83. [ Links ]
93. Sauerland S, Korenkov M, Kleinen T, Arndt M, Paul A. Obesity is a risk factor for recurrence after incisional hernia repair. Hernia. 2004;8(1):42-46. [ Links ]
94. Kirby JP, Mazuski JE. Prevention of surgical site infection. Surg Clin North Am. 2009;89(2):365-389. [ Links ]
95. Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70(3):195-283. [ Links ]
96. Zanetti G, Giardina R, Platt R. Intraoperative redosing of cefazolin and risk for surgical site infection in cardiac surgery. Emerg Infect Dis. 2001;7(5):828-831. [ Links ]
97. Jacobson B, Louw S, Büller H, et al. Venous thromboembolism: Prophylactic and therapeutic practice guideline. SAMJ. 2013;103(4):261-267. [ Links ]
98. Holzheimer R. Laparoscopic procedures as a risk factor of deep venous thrombosis, superficial ascending thrombophlebitis and pulmonary embolism-case report and review of the literature. Eur J Med Res. 2004;9(9):417-422. [ Links ]
99. Tzovaras G, Zacharoulis D, Georgopoulou S, Pratsas K, Stamatiou G, Hatzitheofilou C. Laparoscopic ventral hernia repair under spinal anesthesia: A feasibility study. Am J Surg. 2008;196(2):191-194. [ Links ]
100. Donati M, Brancato G, Donati A. Open incisional hernia repair under local anaesthesia. Acta Chir Belg. 2010;110(1):45-50. [ Links ]
101. Brown C, Finch J. Which mesh for hernia repair? Ann R Coll Surg Engl. 2010;92(4):272-278. [ Links ]
102. Jenkins ED, Yom V, Melman L, et al. Prospective evaluation of adhesion characteristics to intraperitoneal mesh and adhesiolysis-related complications during laparoscopic re-exploration after prior ventral hernia repair. Surg Endosc. 2010;24(12):3002-3007. [ Links ]
103. Shankaran V, Weber DJ, Reed RL 2nd, Luchette FA. A review of available prosthetics for ventral hernia repair. Ann Surg. 2011;253(1):16-26. [ Links ]
104. Eriksen J, Gögenur I, Rosenberg J. Choice of mesh for laparoscopic ventral hernia repair. Hernia. 2007;11(6):481-492. [ Links ]
105. Deeken CR, Faucher KM, Matthews BD. A review of the composition, characteristics, and effectiveness of barrier mesh prostheses utilized for laparoscopic ventral hernia repair. Surg Endosc. 2012;26(2):566-575. [ Links ]
106. Huber A, McCabe GP, Boruch AV, Medberry C, Honerlaw M, Badylak SF. Polypropylene-containing synthetic mesh devices in soft tissue repair: A meta-analysis. J Biomed Mater R B: Appl Biomater. 2012;100(1):145-154. [ Links ]
107. Chowbey P, Sharma A, Khullar R, Mann V, Baijal M, Vashistha A. Laparoscopic ventral hernia repair. J Laparoendosc Adv Surg Tech. 2000;10(2):79-84. [ Links ]
108. Carbonell AM, Criss CN, Cobb WS, Novitsky YW, Rosen MJ. Outcomes of synthetic mesh in contaminated ventral hernia repairs. J Am Coll Surg. 2013;217(6):991-998. [ Links ]
109. Sartelli M, Coccolini F, Van Ramshorst GH, et al. WSES guidelines for emergency repair of complicated abdominal wall hernias. World J Emerg Surg. 2013;8(1):1. [ Links ]
110. Choi JJ, Palaniappa NC, Dallas KB, Rudich TB, Colon MJ, Divino CM. Use of mesh during ventral hernia repair in clean- contaminated and contaminated cases: Outcomes of 33,832 cases. Ann Surg. 2012;255(1):176-180. [ Links ]
111. Harth KC, Rosen MJ. Major complications associated with xenograft biologic mesh implantation in abdominal wall reconstruction. Surg Innov. 2009;16(4):324-329. [ Links ]
112. Cevasco M, Itani KM. Ventral hernia repair with synthetic, composite, and biologic mesh: Characteristics, indications, and infection profile. Surg Infect. 2012;13(4):209-215. [ Links ]
113. Franklin Jr ME, Trevino JM, Portillo G, Vela I, Glass JL, Gonzalez JJ. The use of porcine small intestinal submucosa as a prosthetic material for laparoscopic hernia repair in infected and potentially contaminated fields: Long-term follow-up. Surg Endosc. 2008;22(9):1941-1946. [ Links ]
114. Itani KM, Hur K, Kim LT, et al. Comparison of laparoscopic and open repair with mesh for the treatment of ventral incisional hernia: A randomized trial. Arch Surg. 2010;145(4):322-328. [ Links ]
115. Luijendijk RW, Hop WC, van den Tol, M Petrousjka, et al. A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med. 2000;343(6):392-398. [ Links ]
116. Rosen MJ, Krpata DM, Ermlich B, Blatnik JA. A 5-year clinical experience with single-staged repairs of infected and contaminated abdominal wall defects utilizing biologic mesh. Ann Surg. 2013;257(6):991-996. [ Links ]
117. Bellows CF, Smith A, Malsbury J, Helton WS. Repair of incisional hernias with biological prosthesis: A systematic review of current evidence. Am J Surg. 2013;205(1):85-101. [ Links ]
118. Huerta S, Varshney A, Patel PM, Mayo HG, Livingston EH. Biological mesh implants for abdominal hernia repair: US food and drug administration approval process and systematic review of its efficacy. JAMA Surg. 2016;151(4):374-381. [ Links ]
119. DeNoto G, Reaven N, Funk S. Ventral hernia: Retrospective cost analysis of primary repair, repair with synthetic mesh, and repair with acellular xenograft implant. Open Access Surg. 2013;6:23-32. [ Links ]
120. Catena F, Coccolini F, Ansaloni L, Di Saverio S, Pinna A. Closure of the LAPSIS trial (Br J Surg 2010; 97: 1598). Br J Surg. 2011;98(2):319-319. [ Links ]
121. Miserez M, Grass G, Weiss C, Stützer H, Sauerland S, Neugebauer E. Your views. 2010. [ Links ]
122. Cobb GA, Shaffer J. Cross-linked acellular porcine dermal collagen implant in laparoscopic ventral hernia repair: Case-controlled study of operative variables and early complications. Int Surg. 2005;90(3 Suppl):S24-9. [ Links ]
123. Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg. 2004;240(4):578-585. [ Links ]
124. Schumacher OP, Peiper C, Lorken M, Schumpelick V. Long- term results after Spitzy's umbilical hernia repair. Chirurg. 2003;74(1):50-54. [ Links ]
125. den Hartog D, Dur AH, Tuinebreijer WE, Kreis RW. Open surgical procedures for incisional hernias. Cochrane Libr. 2008. [ Links ]
126. Christoffersen MW, Helgstrand F, Rosenberg J, Kehlet H, Strandfelt P, Bisgaard T. Long-term recurrence and chronic pain after repair for small umbilical or epigastric hernias: A regional cohort study. Am J Surg. 2015;209(4):725-732. [ Links ]
127. Nguyen MT, Berger RL, Hicks SC, et al. Comparison of outcomes of synthetic mesh vs suture repair of elective primary ventral herniorrhaphy: A systematic review and meta-analysis. JAMA Surg. 2014;149(5):415-421. [ Links ]
128. Aslani N, Brown C. Does mesh offer an advantage over tissue in the open repair of umbilical hernias? A systematic review and meta-analysis. Hernia. 2010;14(5):455-462. [ Links ]
129. Arroyo A, Garcia P, Perez F, Andreu J, Candela F, Calpena R. Randomized clinical trial comparing suture and mesh repair of umbilical hernia in adults. Br J Surg. 2001;88(10):1321-1323. [ Links ]
130. Winsnes A, Haapamäki M, Gunnarsson U, Strigárd K. Surgical outcome of mesh and suture repair in primary umbilical hernia: Postoperative complications and recurrence. Hernia. 2016:1-8. [ Links ]
131. Venclauskas L, Silanskaite J, Kiudelis M. Umbilical hernia: Factors indicative of recurrence. Medicina (Kaunas). 2008;44(11):855-859. [ Links ]
132. Dur A, den Hartog D, Tuinebreijer W, Kreis R, Lange J. Low recurrence rate of a two-layered closure repair for primary and recurrent midline incisional hernia without mesh. Hernia. 2009;13(4):421-426. [ Links ]
133. Abdel-Baki N, Bessa S, Abdel-Razek A. Comparison of prosthetic mesh repair and tissue repair in the emergency management of incarcerated para-umbilical hernia: A prospective randomized study. Hernia. 2007;11(2):163-167. [ Links ]
134. Christoffersen MW, Helgstrand F, Rosenberg J, Kehlet H, Bisgaard T. Lower reoperation rate for recurrence after mesh versus sutured elective repair in small umbilical and epigastric hernias. A nationwide register study. World J Surg. 2013;37(11):2548-2552. [ Links ]
135. Eryilmaz R, Sahin M, Tekelioglu MH. Which repair in umbilical hernia of adults: Primary or mesh? Int Surg. 2006;91(5):258-261. [ Links ]
136. Funk LM, Perry KA, Narula VK, Mikami DJ, Melvin WS. Current national practice patterns for inpatient management of ventral abdominal wall hernia in the United States. Surg Endosc. 2013;27(11):4104-4112. [ Links ]
137. Rogmark P, Petersson U, Bringman S, et al. Short-term outcomes for open and laparoscopic midline incisional hernia repair: A randomized multicenter controlled trial: The ProLOVE (prospective randomized trial on open versus laparoscopic operation of ventral eventrations) trial. Ann Surg. 2013;258(1):37-45. [ Links ]
138. Poelman M, Apers J, van den Brand H, et al. The INCH-trial: A multicentre randomized controlled trial comparing the efficacy of conventional open surgery and laparoscopic surgery for incisional hernia repair. BMC surgery. 2013;13(1):1. [ Links ]
139. Zhang Y, Zhou H, Chai Y, Cao C, Jin K, Hu Z. Laparoscopic versus open incisional and ventral hernia repair: A systematic review and meta-analysis. World J Surg. 2014;38(9):2233-2240. [ Links ]
140. Al Chalabi H, Larkin J, Mehigan B, McCormick P. A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Int J Surg. 2015;20:65-74. [ Links ]
141. Awaiz A, Rahman F, Hossain M, et al. Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Hernia. 2015;19(3):449-463. [ Links ]
142. Stirler VM, Schoenmaeckers EJ, de Haas RJ, Raymakers JT, Rakic S. Laparoscopic repair of primary and incisional ventral hernias: The differences must be acknowledged. Surg Endosc. 2014;28(3):891-895. [ Links ]
143. Kockerling F, Schug-Pass C, Adolf D, Reinpold W, Stechemesser B. Is pooled data analysis of ventral and incisional hernia repair acceptable? Front Surg. 2015;2:15. [ Links ]
144. Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M. Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Libr. 2011. [ Links ]
145. Arita NA, Nguyen MT, Nguyen DH, et al. Laparoscopic repair reduces incidence of surgical site infections for all ventral hernias. Surg Endosc. 2015;29(7):1769-1780. [ Links ]
146. Forbes S, Eskicioglu C, McLeod R, Okrainec A. Meta-analysis of randomized controlled trials comparing open and laparoscopic ventral and incisional hernia repair with mesh. Br J Surg. 2009;96(8):851-858. [ Links ]
147. Kaafarani HM, Hur K, Hirter A, et al. Seroma in ventral incisional herniorrhaphy: Incidence, predictors and outcome. Am J Surg. 2009;198(5):639-644. [ Links ]
148. Meyer R, Häge A, Zimmermann M, et al. Is laparoscopic treatment of incisional and recurrent hernias associated with an increased risk for complications? Int J Surg. 2015;19:121-127. [ Links ]
149. Rogmark P, Petersson U, Bringman S, Ezra E, Osterberg J, Montgomery A. Quality of life and surgical outcome 1 year after open and laparoscopic incisional hernia repair: ProLOVE: A randomized controlled trial. Ann Surg. 2016;263(2):244-250. [ Links ]
150. Ecker BL, Kuo LE, Simmons KD, Fischer JP, Morris JB, Kelz RR. Laparoscopic versus open ventral hernia repair: Longitudinal outcomes and cost analysis using statewide claims data. Surg Endosc. 2016;30(3):906-915. [ Links ]
151. Misra M, Bansal V, Kulkarni M, Pawar D. Comparison of laparoscopic and open repair of incisional and primary ventral hernia: Results of a prospective randomized study. Surg Endosc And Other Interventional Techniques. 2006;20(12):1839-1845. [ Links ]
152. Olmi S, Scaini A, Cesana G, Erba L, Croce E. Laparoscopic versus open incisional hernia repair. Surg Endosc. 2007;21(4):555-559. [ Links ]
153. Colavita PD, Tsirline VB, Belyansky I, et al. Prospective, long term comparison of quality of life in laparoscopic versus open ventral hernia repair. Ann Surg. 2012;256(5):714-22; discussion 722-3. [ Links ]
154. Liang MK, Clapp M, Li LT, Berger RL, Hicks SC, Awad S. Patient satisfaction, chronic pain, and functional status following laparoscopic ventral hernia repair. World J Surg. 2013;37(3):530-537. [ Links ]
155. American hernia society. https://americanherniasociety.org/resources-for-surgeons/video-library/. Accessed 22 August 2016. [ Links ]
156. Nguyen DH, Nguyen MT, Askenasy EP, Kao LS, Liang MK. Primary fascial closure with laparoscopic ventral hernia repair: Systematic review. World J Surg. 2014;38(12):3097-3104. [ Links ]
157. Earle D, Roth JS, Saber A, et al. SAGES guidelines for laparoscopic ventral hernia repair. Surg Endosc. 2016;30(8):3163-3183. [ Links ]
158. Vorst AL, Kaoutzanis C, Carbonell AM, Franz MG. Evolution and advances in laparoscopic ventral and incisional hernia repair. WJGS. 2015;7(11):293. [ Links ]
159. Rosen MJ, Fatima J, Sarr MG. Repair of abdominal wall hernias with restoration of abdominal wall function. JGS. 2010;14(1):175-185. [ Links ]
160. Palanivelu C, Jani K, Senthilnathan P, Parthasarathi R, Madhankumar M, Malladi V. Laparoscopic sutured closure with mesh reinforcement of incisional hernias. Hernia. 2007;11(3):223-228. [ Links ]
161. Chelala E, Baraké H, Estievenart J, Dessily M, Charara F, Allé J. Long-term outcomes of 1326 laparoscopic incisional and ventral hernia repair with the routine suturing concept: A single institution experience. Hernia. 2016;20(1):101-110. [ Links ]
162. Clapp ML, Hicks SC, Awad SS, Liang MK. Trans-cutaneous closure of central defects (TCCD) in laparoscopic ventral hernia repairs (LVHR). World J Surg. 2013;37(1):42-51. [ Links ]
163. Colak E, Ozlem N, Kucuk GO, Aktimur R, Kesmer S, Yildirim K. Prospective randomized trial of mesh fixation with absorbable versus nonabsorbable tacker in laparoscopic ventral incisional hernia repair. Int J Clin Exp Med. 2015;8(11):21611-21616. [ Links ]
164. Nguyen SQ, Divino CM, Buch KE, et al. Postoperative pain after laparoscopic ventral hernia repair: A prospective comparison of sutures versus tacks. JSLS. 2008;12(2):113-116. [ Links ]
165. Sajid MS, Parampalli U, McFall MR. A meta-analysis comparing tacker mesh fixation with suture mesh fixation in laparoscopic incisional and ventral hernia repair. Hernia. 2013;17(2):159-166. [ Links ]
166. Holihan JL, Nguyen DH, Nguyen MT, Mo J, Kao LS, Liang MK. Mesh location in open ventral hernia repair: A systematic review and network meta-analysis. World J Surg. 2016;40(1):89-99. [ Links ]
167. Albino FP, Patel KM, Nahabedian MY, Sosin M, Attinger CE, Bhanot P. Does mesh location matter in abdominal wall reconstruction? A systematic review of the literature and a summary of recommendations. Plast Reconstr Surg. 2013;132(5):1295-1304. [ Links ]
168. Deerenberg E, Timmermans L, Hogerzeil D, et al. A systematic review of the surgical treatment of large incisional hernia. Hernia. 2015;19(1):89-101. [ Links ]
169. Eriksson A, Rosenberg J, Bisgaard T. Surgical treatment for giant incisional hernia: A qualitative systematic review. Hernia. 2014;18(1):31-38. [ Links ]
170. LeBlanc KA, Elieson MJ, Corder JM. Enterotomy and mortality rates of laparoscopic incisional and ventral hernia repair: A review of the literature. JSLS. 2007;11(4):408-414. [ Links ]
171. Sharma A, Khullar R, Soni V, et al. Iatrogenic enterotomy in laparoscopic ventral/incisional hernia repair: A single center experience of 2,346 patients over 17 years. Hernia. 2013;17(5):581-587. [ Links ]
172. Aguilar B, Chapital AB, Madura JA, Harold KL. Conservative management of mesh-site infection in hernia repair. J Laparoendosc Adv Surg Tech. 2010;20(3):249-252. [ Links ]
173. Silecchia G, Campanile FC, Sanchez L, et al. Laparoscopic ventral/incisional hernia repair: Updated guidelines from the EAES and EHS endorsed consensus development conference. Surg Endosc. 2015;29(9):2463-2484. [ Links ]
174. Brown RH, Subramanian A, Hwang CS, Chang S, Awad SS. Comparison of infectious complications with synthetic mesh in ventral hernia repair. Am J Surg. 2013;205(2):182-187. [ Links ]
175. Berrevoet F, Vanlander A, Sainz-Barriga M, Rogiers X, Troisi R. Infected large pore meshes may be salvaged by topical negative pressure therapy. Hernia. 2013;17(1):67-73. [ Links ]
176. Chatzoulis G, Chatzoulis K, Spyridopoulos P, Pappas P, Ploumis A. Salvage of an infected titanium mesh in a large incisional ventral hernia using medicinal honey and vacuum-assisted closure: A case report and literature review. Hernia. 2012;16(4):475-479. [ Links ]
177. Tsimoyiannis EC, Siakas P, Glantzounis G, Koulas S, Mavridou P, Gossios KI. Seroma in laparoscopic ventral hernioplasty. Surg Laparosc Endosc Percutan Tech. 2001;11(5):317-321. [ Links ]
178. Castro PM, Rabelato JT, Monteiro GG, Guerra G, Mazzurana M, Alvarez GA. Laparoscopy versus laparotomy in the repair of ventral hernias: Systematic review and meta-analysis. Arq Gastroenterol. 2014;51(3):205-211. [ Links ]
179. Sajid MS, Bokhari SA, Mallick AS, Cheek E, Baig MK. Laparoscopic versus open repair of incisional/ventral hernia: A meta-analysis. Am J Surg. 2009;197(1):64-72. [ Links ]
180. Heniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic repair of ventral hernias: Nine years' experience with 850 consecutive hernias. Ann Surg. 2003;238(3):391-400. [ Links ]
181. Carbonell AM, Harold KL, Mahmutovic AJ, Hassan R. Local injection for the treatment of suture site pain after laparoscopic ventral hernia repair. Am Surg. 2003;69(8):688. [ Links ]
182. Majeski J. Open and laparoscopic repair of Spigelian hernia. Int Surg. 2009;94(4):365-369. [ Links ]
183. Hilling DE, Koppert LB, Keijzer R, Stassen LP, Oei IH. Laparoscopic correction of umbilical hernias using a transabdominal preperitoneal approach: Results of a pilot study. Surg Endosc. 2009;23(8):1740-1744. [ Links ]
184. Tarnoff M, Rosen M, Brody F. Planned totally extraperitoneal laparoscopic spigelian hernia repair. Surg Endosc and Other Interventional Techniques. 2002;16(2):359-359. [ Links ]
185. Koksal N, Altinli E, Celik A, Oner I. Extraperitoneal laparoscopic approach to Spigelian hernia combined with groin hernias. Surg Laparosc Endosc Percutan Tech. 2004;14(4):204-206. [ Links ]
186. Bhandarkar DS, Katara AN, Shah RS, Udwadia TE. Transabdominal preperitoneal repair of a port-site incisional hernia. J Laparoendosc Adv Surg Tech. 2005;15(1):60-62. [ Links ]
187. Ramirez OM, Ruas E, Dellon AL. "Components separation" method for closure of abdominal-wall defects: An anatomic and clinical study. Plast Reconstr Surg. 1990;86(3):519-526. [ Links ]
188. Rosen M, Jin J, McGee M, Williams C, Marks J, Ponsky J. Laparoscopic component separation in the single-stage treatment of infected abdominal wall prosthetic removal. Hernia. 2007;11(5):435-440. [ Links ]
189. Harth KC, Rosen MJ. Endoscopic versus open component separation in complex abdominal wall reconstruction. Am J Surg. 2010;199(3):342-347. [ Links ]
190. Petro CC, Posielski NM, Raigani S, Criss CN, Orenstein SB, Novitsky YW. Risk factors for wound morbidity after open retromuscular (sublay) hernia repair. Surg. 2015;158(6):1658-1668. [ Links ]
191. Krpata DM, Blatnik JA, Novitsky YW, Rosen MJ. Posterior and open anterior components separations: A comparative analysis. Am J Surg. 2012;203(3):318-322. [ Links ]
192. Pauli EM, Rosen MJ. Open ventral hernia repair with component separation. Surg Clin North Am. 2013;93(5):1111-1133. [ Links ]
193. Gould JC, Ellison EC. Laparoscopic parastomal hernia repair. Surg Laparosc Endosc Percutan Tech. 2003;13(1):51-54. [ Links ]
194. Sugarbaker PH. Peritoneal approach to prosthetic mesh repair of paraostomy hernias. Ann Surg. 1985;201(3):344-346. [ Links ]
195. Hansson B, Bleichrodt R, De Hingh I. Laparoscopic parastomal hernia repair using a keyhole technique results in a high recurrence rate. Surg Endosc. 2009;23(7):1456-1459. [ Links ]
196. Berger D, Bientzle M. Laparoscopic repair of parastomal hernias: A single surgeon's experience in 66 patients. Dis Colon Rectum. 2007;50(10):1668-1673. [ Links ]
197. Morris-Stiff G, Hughes LE. The continuing challenge of parastomal hernia: Failure of a novel polypropylene mesh repair. Ann R Coll Surg Eng. 1998;80(3):184-187. [ Links ]
198. Jänes A, Cengiz Y, Israelsson LA. Preventing parastomal hernia with a prosthetic mesh: A 5-year follow-up of a randomized study. World J Surg. 2009;33(1):118-121. [ Links ]
199. Serra-Aracil X, Bombardo-Junca J, Moreno-Matias J, et al. Randomized, controlled, prospective trial of the use of a mesh to prevent parastomal hernia. Ann Surg. 2009;249(4):583-587. [ Links ]
200. Wijeyekoon SP, Gurusamy K, El-Gendy K, Chan CL. Prevention of parastomal herniation with biologic/composite prosthetic mesh: A systematic review and meta-analysis of randomized controlled trials. J Am Coll Surg. 2010;211(5):637-645. [ Links ]
201. Akram J, Matzen SH. Rectus abdominis diastasis. J Plast Surg Hand Surg. 2014;48(3):163-169. [ Links ]
202. Nahas FX, Augusto SM, Ghelfond C. Should diastasis recti be corrected? Aesthetic Plast Surg. 1997;21(4):285-289. [ Links ]
 Correspondence:
Correspondence:
Dr Ravi Oodit
ravio@surgcare.co.za













