Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.115 n.9 Pretoria Oct. 2025
https://doi.org/10.7196/SAMJ.2025.v115i9.3049
RESEARCH
Wound documentation by doctors in academic emergency departments, Gauteng Province, South Africa
R KleynhansI; J du PlessisII; P MoodleyII
IMB ChB, DipPEC (SA); Division of Emergency Medicine, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIMB ChB, FCEM (SA); Division of Emergency Medicine, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. Medical doctors manage trauma cases daily, most needing medicolegal documentation. Wound documentation is a vital skill required by doctors.
OBJECTIVES. To describe and compare the knowledge and practices of documentation of clinical findings on the J88 form, looking at the accuracy of wound features and wound size estimation, focusing on participant gender, medical level of experience and type of injury simulated.
METHODS. This was a multi-centre, prospective, observational, cross-sectional study of three academic emergency departments in the University of the Witwatersrand academic circuit using questionnaires, moulage and wound characteristic rubrics.
RESULTS. Eighty-three doctors participated in the study. This was equally spread between sexes. According to wound rubrics, participants scored an average of 48% for accuracy of J88 form completion. The most precise wound description was abrasion (62.5%). The least precise wound description was stab wound (33.3%). Most participants (63.8%) noted on the questionnaire that they always indicate bruises; however, 25.3% missed the simulated bruise. The most frequently documented wound features were location and size estimation (98.8%). The least documented wound feature was the age and mechanism of the injury (<6%). Large wounds (>5 cm length) were underestimated (p<0.001), with accurate size estimations of smaller wounds (<5 cm). Perceptions of undergraduate training in wound documentation were evenly divided between acceptable and poor, while postgraduate training was generally regarded as poor.
CONCLUSION. This study found that wound documentation among emergency department doctors was poor, with participants scoring an average of 48% across the marking rubric. More training at both undergraduate and postgraduate levels is recommended.
Keywords: wound documentation, form J88, medicolegal documentation, emergency department, interpersonal violence
'There is a kind of medical knowledge which is not so much concerned with the cure of disease as the detection of error and the conviction of guilt' - Samuel Farr, 1788
The trauma crisis in South Africa (SA) is witnessed daily by doctors working in emergency departments (EDs).[1-8] KwaZulu-Natal (KZN) and the Western Cape are the only provinces in SA with electronic trauma registries.[1,4] A KZN study of data from one of these electronic registries found 1 263 847 ED visits for assault, gunshots and motor vehicle accidents from 2012 to 2022.[1] Intentional trauma exceeds non-intentional trauma with a ratio of 2:1.[1] A single-centre study in the Eastern Cape Province found that 42.2% of trauma-related ED visits were due to interpersonal violence (IPV).[2]
Doctors are not only responsible for treating victims of IPV, but also need to record injuries to aid as evidence in legal investigations.[5-9] The J88 form is a medicolegal document from the Department of Justice, and is unique to SA.[6,8] The first attending medical practitioner completes it.[8] Kotzé et al.[8,9] and Müller et al.[6] have published articles with guidelines outlining how to complete the J88 form, aiming to improve documentation. Multiple studies have emphasised the importance of accurate documentation and its effect on criminal prosecution.[5-10]
In a sensory ethnographic study by Mogale et al.,[10] prosecutors stated the following: '(The) J88 is real and conclusive evidence because it is presented under Section 212 of the Criminal Procedure Act as amended'. Additionally, prosecutors stated that medical practitioners were not completing the J88 forms accurately.[10]
A 2018 study of community service medical officers (CSOs) who had graduated from the University of the Free State (UFS) drew attention to their lack of training on medicolegal documentation. Only 26.8% of participants reported having had undergraduate training on completing the J88 form for assault cases.[7] This highlighted the knowledge gap experienced by doctors regarding adequate medicolegal documentation.[7]
This study aimed to assess the accuracy of wound documentation by doctors working in mixed medical and trauma EDs based on clinical findings documented on the J88 form, according to a simulated scenario.
Methods
Design
This multi-centre prospective, observational, cross-sectional study was approved by the University of the Witwatersrand Human Research Ethics Committee (ref. no. M230251). The population size was estimated at 100 doctors. For a confidence level of 95% and a margin of error of 5%, the convenience sample size was approximated at 80 doctors.
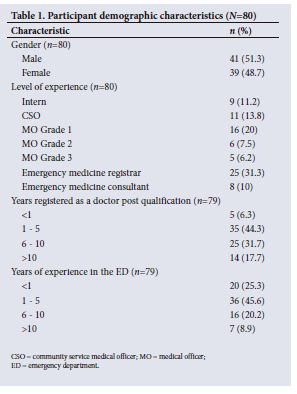
The study population comprised emergency medicine consultants and registrars, medical officers (MOs), community service medical officers (CSOs) and medical interns. Years post qualification as independent medical practitioners categorise medical officers.
Grade 1 medical officers (MO 1) have <5 years' work experience, grade 2 medical officers (MO 2) have 5 - 10 years' experience, and grade 3 medical officers have >10 years' experience.
Study sites included Helen Joseph Tertiary Hospital and two regional hospitals: Tambo Memorial Hospital and Thelle Mogoerane Regional Hospital. All three hospitals have mixed EDs with large trauma burdens.
Data collection
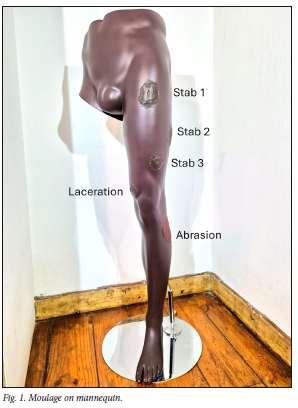
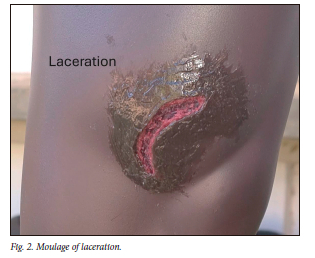
Moulage of various injuries was made by the primary investigator using silicone and a clothing mannequin limb (Fig. 1). Six injuries were depicted: three stab wounds, one laceration, one bruise and one abrasion (Figs 1, 2 and 3). Basic terminology included:

• stab: a sharp force injury that is deeper than long[7]
• laceration: an open wound from blunt force injuries caused by tearing of the skin[7]
• bruise: blunt force trauma applied to an area resulting in rupture of the capillary blood vessels in the underlying soft tissue[7]
• abrasion: blunt force injury to superficial layers of the skin, scraping the surface of the skin.[7]
All injuries were described, measured and validated by two specialist emergency physicians and one trauma surgeon. A station was set up with the mannequin, and a short clinical scenario was given to the participants. An information sheet was supplied to each participant. Informed consent was implied by the completion of the questionnaire and J88 form. Participants were requested to complete a questionnaire and document injuries (as simulated by moulage on the mannequin) on a J88 form (appendix, http://coding.samedical.org/file/2370). Sections of the J88 form given for completion by participants were the clinical findings of section F (appendix A), and the anatomical diagrams (appendix B).
The questionnaire consisted of basic demographics, experience in the ED, how often participants manage IPV, frequency of J88 form completion, documentation of wound characteristics and participants' impression of undergraduate and postgraduate training on wound documentation and measurement.
Assessment of wound documentation
Wound documentation relating to demographics was analysed according to the total number of participants who completed the relevant question of the questionnaire. Wound documentation on the J88 form that did not relate to demographics was analysed according to the total number of participants who completed the J88 form.
Completed J88 pages were marked against a pre-set validated rubric for each wound (appendix C). The rubric was based on that produced in a study by Loots et al. (appendix D).[5] Each rubric assessed specific wound characteristics: type of injury, wound description (location, size, shape, age estimation), mechanism, and correlation of wound description to the anatomical diagram. A rubric was compiled for stab wounds, incisions and lacerations, with a total score of nine. A separate rubric was compiled for abrasions and bruises, with a total score of eight. These weighted scores contributed to a global mark representing the accuracy of wound documentation across blunt and sharp force injuries, as well as the overall accuracy of wound documentation. Data were collected over 3 months from July 2023 to September 2023.
Data analysis
Data were analysed by an external statistician with IBM SPSS Statistics version 28 (IBM, USA). Descriptive statistics are presented as frequencies and percentages for categorical variables, and as means (standard deviations) or medians (interquartile ranges) for continuous scale variables. Where data were skewed, comparisons were done using the Kruskal-Wallis test. The sample t-test was used to examine for under- and overestimation. Significance testing was done using ANOVA for normal distributed data. Statistical significance was accepted as a p<0.05.
Results
Demographics
Eighty-three participants completed the J88 form, and 80 completed the questionnaire. Three participants gave no reason why they did not complete the questionnaire. Demographics are documented in Table 1.
Current practices on wound documentation
Participants rated their usual practice in terms of several aspects of wound documentation, from 'never' to 'always.' Most participants self-reported that they 'always' document lacerations (82.5%), bruises (63.8%) and abrasions (62.5%), with little variability between participants' answers. While 71.8% of participants stated that they 'always' document stab wounds, 2.6% indicated that they 'sometimes' indicate these, 3.8% 'rarely' and 1.3% of participants indicated 'never'. Participant answers had high variability ranging from 'never' to 'always'. Most participants (72.5%) reported that they 'always' document incisions, 2.5% 'never' document incisions and 7.5% stated that they did so 'rarely'.
Most participants (42.5%) indicated that wound measurement is 'always' important, although they 'never' (20%), 'rarely' (41.3%) and 'sometimes' (35%) measure wounds to ensure accuracy.
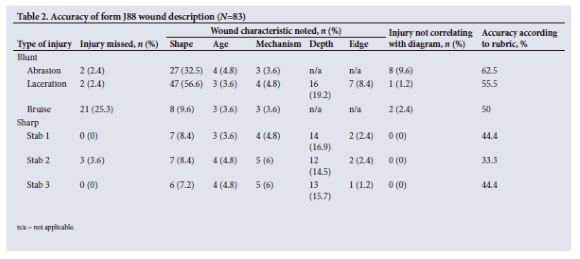
Wound description of simulated injuries
According to the pre-set rubric, the average overall accuracy of wound documentation was 48%. The overall score for blunt force injuries was an average of 56%, and sharp force injuries scored 40.7%. The accuracy of individual wound documentation was as follows: abrasion, 62.5%; laceration, 55.5%; bruise, 50%; stabs 1 and 3, 44.4%; and stab 2, 33.3%. The location and size of the wound were documented by 98.8% (n=82) of participants across all wounds. (Table 2).
Most participants (89.2%, n=74) correctly signed pages 4 and 6 of the J88 form. One participant described an additional wound that was not part of the wound moulage.
There was no statistically significant relationship between qualification, years qualified as a doctor and years of experience in the ED in improved wound documentation.
Wound size estimations
Wound size was underestimated in most large wounds (>5 cm length), but accurate in smaller wounds. There was a statistically significant underestimation of abrasion length (p<0.001), abrasion width (p<0.001), bruise length (p<0.001) and laceration length (p<0.001). Blunt force injuries were underestimated, while sharp force injuries were accurate to within 2 mm (Table 3).
Subgroup analysis of wound size estimations
There were no statistically significant differences between sexes, qualifications, or years since qualification as a medical practitioner.
Perception of training
Likert scale analysis was done, with a focus on central tendency. Wound documentation training during undergraduate education was considered either 'poor' or 'acceptable' by 30% each of participants, 'very poor' by 18.8% and 'very good' by only 2.5%. Postgraduate wound documentation training was considered 'very poor' (34.2%) or 'poor' (43.4%) by most participants, with only 10.5% finding it 'acceptable', 9.2% 'good' and 2.6% 'very good'.
Both undergraduate and postgraduate training in wound measurement was considered 'poor' or 'very poor' (70.5% and 84%, respectively).
Discussion
Trauma is a widespread issue in SA, placing significant demands on both medical and legal systems.[1,5,6] The J88 form provides the judicial system with medical evidence, and the doctor's interpretation of injuries.[5-10] Information obtained from the J88 form is more useful to the justice process when the documentation is complete and accurate.[5-9] Proper wound description - including location, size, shape, depth, edge and age - requires sound medical terminology and adequate training.[5-9]
Training gaps persist. Most study participants expressed that undergraduate training in wound documentation was 'acceptable' or 'poor', with postgraduate training as largely 'poor'. Fouché et al.[7] found that while >65% of UFS medical school graduates had had prior training in general medicolegal and wound documentation, >73% had not received training specific to J88 completion. Training encompasses medicolegal documentation in terms of overall accuracy and specific wound features.
Documentation remains poor. In our study, the overall average accuracy of wound documentation was 48%. These findings echoed those of a Pretoria study, where <20% of cases were appropriately documented.[5]
Interestingly, our study found that the description of blunt force injuries scored higher than that of sharp force injuries. This could be attributed to the study design and the Hawthorne effect. Other studies found that blunt force injuries were often missed or inadequately described.[5,7] Caution must be used when interpreting these data, as further studies are needed on the discrepancy between blunt and sharp force injuries.
Despite the improved scoring of blunt force injuries, a sizeable proportion of bruises in our study were missed (25.3%), and it remains unclear whether including them would have improved scores. Blunt and sharp force injuries have specific characteristics that set them apart.[6] Documentation of positive features may allow identification of the weapon of assault.[6]
Descriptions lacked key details. While participants self-reported that they often described the shape of injuries, <10% of participants indicated the shape of sharp force injuries. Age and suspected mechanism of injury were recorded in <6% of injuries. These findings are consistent with those of Loots et al.,[5] who also noted that specific wound characteristics, such as shape and age, were rarely documented.
Perceived competence often exceeds actual performance, reflecting the Dunning-Kruger effect. Contributing factors include lack of knowledge, time constraints and the absence of feedback mechanisms, as the J88 forms are not routinely audited.[5]
Our study found that the most frequently documented wound features (98.8%) were location and size. Again, Loots et al.[5] had similar findings, with >50% of injury documentation indicating location.Our study found that large wounds (>5 cm length) were underestimated, while size estimation was more accurate for wounds <5 cm (within 2 mm accuracy).
A UK study found that consultants had larger error proportions, and that sex influenced wound size estimation, with males overestimating and females underestimating wound sizes.[11] The authors speculated that junior staff were directly involved in acute wound management, but did not explain why sexes differ.[11] Sex and level of experience did not play a role in improved wound documentation or wound size estimation in our study - possibly due to greater trauma exposure in SA.
Medicolegal documentation is an essential skill, yet as Mogale et al.[10] state, doctors document from a health and not a legal perspective.
Current training is inadequate to equip doctors in the specialised field of medicolegal documentation and legal proceedings of the justice system.[5-8,10] Improved education, clearer protocols, templates, measuring tools and continuing professional development initiatives are needed.[5,11,12] Enhancing undergraduate training is key to preparing junior doctors to care for victims of IPV.[5,7,10]
Study limitations
This was a small study. It was performed in academic regional and tertiary hospitals, and may not be reflective of the practices at smaller hospitals and community health centres. Convenience sampling was used.
Dissemination of results
The results of this study will be shared with the Division of Emergency Medicine at the University of the Witwatersrand. The study and its findings will be presented at future academic meetings, and forwarded to the participating EDs.
Conclusion
Wound documentation is a vital skill that requires more training at both undergraduate and postgraduate levels. It is necessary to address this skill deficit, and improve accurate medicolegal documentation. Implementing wound description templates and the use of measuring devices in EDs may improve documentation, and should be investigated in future studies.
Data availability. Data available from authors on reasonable request.
Declaration. This publication was a requirement for RK's MMed (Emergency Medicine) degree from the University of the Witwatersrand.
Acknowledgements. To Robin Burrow for his continued support during this study.
Author contributions. RK 60%; JdP 20%; PM 20%.
Funding. None.
Conflicts of interest. None.
References
1. Tefera A, Lutge EE, Moodley N, et al. Tracking the trauma epidemic in KwaZulu-Natal, South Africa. World J Surg 2023;47(8):1940-1945. https://doi.org/10.1007/s00268-023-07032-2 [ Links ]
2. Mitra A, Okafor UB, Kaswa R, Adeniyi OV. Epidemiology of interpersonal violence at a regional hospital emergency unit in Eastern Cape, South Africa. S Afr Fam Pract 2022;64(1)e1-e5. https://doi.org/10.4102/safp.v64i1.5511 [ Links ]
3. Hardcastle T, Oosthuizen G, Clarke D, Lutge E. Trauma, a preventable burden of disease in South Africa: Review of the evidence, with a focus on KwaZulu-Natal. In: Padarath A, King J, Mackie E, Casciola J, eds. South African Health Review. Durban: Health Systems Trust, 2016;179-189. [ Links ]
4. Bhana M, Fru P, Plani F. A long walk to freedom: The epidemiology of penetrating trauma in South Africa - analysis of 4 697 patients over a six-year period at Chris Hani Baragwanath Academic Hospital. South Afr J Surg 2022;60(2):77-83. https://doi.org/10.17159/2078-5151/sajs3582 [ Links ]
5. Loots DP, Saayman G. Medicolegal perspectives of interpersonal violence: A review of first-contact clinical notes. S Afr Med J 2019;109(10):792-800. https://doi.org/10.7196/samj.2019.v109i10.13951 [ Links ]
6. Müller K, Saayman G. Clinical forensic medicine: Completing the Form J88 - what to do and what not to do. S Afr Fam Pract 2003;45(8):39-43. https://doi.org/10.4102/safp.v45i8.1886 [ Links ]
7. Fouché L, Bezuidenhout J, Liebenberg C, Adefuye AO. Practice of community-service doctors in the assessment and medico-legal documentation of common physical assault cases. S Afr Fam Pract 2017;60(1):21-25. https://doi.org/10.1080/20786190.2017.1364014 [ Links ]
8. Kotzé JM, Brits H, Botes BA. Part 1: Medico-legal documentation South African Police Service forms, Department of Justice forms and patient information. S Afr Fam Pract 2014;56(5):16-22. [ Links ]
9. Kotzé JM, Brits H, Monatisa MS, Botes J. Part 2: Medico-legal documentation. Practical completion of pages 1 and 4 of the J88 form. S Afr Fam Pract 2014;56(6):32-37. [ Links ]
10. Mogale R, Kushner KE, Richter MS. 'If it is a tear let it be a tear, not a laceration': Form J88 as evidence in prosecution of violence against women in South Africa. Afr Safety Promotion J 2015;13(2):17-30. [ Links ]
11. Peterson N, Stevenson H, Sahni V. Size matters: How accurate is clinical estimation of traumatic wound size? Injury 2014;45(1):232-236. https://doi.org/10.1016/j.injury.2012.04.018 [ Links ]
12. Twaij A, Carballido FC, Maryosh J, Pucher PH. Results of a simple intervention to improve documentation quality in major trauma. Int J Surg 2013;11(8):710. https://doi.org/10.1016/j.ijsu.2013.06.658 [ Links ]
 Correspondence:
Correspondence:
R Kleynhans
rochekleynhans@gmail.com
Received 23 January 2025
Accepted 13 June 2025













