Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309Print version ISSN 1681-150X
SA orthop. j. vol.21 n.3 Centurion 2022
https://doi.org/10.17159/2309-8309/2022/v21n3a2
TRAUMA
Triceps-off transfascial sleeve approach, functional outcomes and surgical technique in distal humerus fractures
Woyisile B NkomoI, *; Pududu A RachueneI; Roopam DeyII; Sithombo MaqungoI; Stephen RocheI; Michael SolomonsI
IGroote Schuur Hospital, Department of Orthopaedic Surgery, University of Cape Town, Cape Town, South Africa
IIDepartment of Human Biology, Department of Surgery, University of Cape Town, Cape Town, South Africa
ABSTRACT
BACKGROUND: We aimed to assess functional and clinical outcomes of patients who underwent open reduction and internal fixation of distal intra-articular fractures of the humerus through a previously undescribed approach through the triceps tendon, called the triceps-off, transfascial sleeve (TOFS) approach
METHODS: We conducted an ambispective cohort study of ten patients who underwent open reduction and internal fixation of the distal humerus through the TOFS approach at a tertiary hospital between March 2016 and January 2019. Patients were identified from the prospectively kept surgical database. All had AO type C fractures of the distal humerus. The mean age was 36.7 ± 14.9 years (range 19-68). The assessment consisted of a review of their hospital records, range of motion, triceps strength, ultrasound evaluation of triceps tendon integrity, X-rays for union rates and adequacy of reduction, and DASH scores
RESULTS: The mean time of follow-up was 10.8 ± 4.7 months (range 6-19). The mean arc of motion was 114.7 ± 25.1 degrees (range 80-150). There was a decrease in mean triceps muscle strength compared to the uninjured side: 66% at 45° of flexion, 70% at 90° and 86% at 120° of elbow flexion. The mean DASH score was 15.7 ± 8.9, indicating mild residual impairment (range 5-31). The DASH score had a strong correlation (r = 0.71; p < 0.05) with the follow-up period. All tendons were intact on ultrasound evaluation. One patient had deep surgical site infection, treated with surgical debridement, antibiotics and plate removal with resolution of sepsis and healing. All fractures united by six months
CONCLUSION: TOFS is a successful surgical approach for reduction and fixation of AO type C intra-articular distal humerus fractures, with excellent tendon healing rates. It is, however, associated with mild residual functional impairment and residual triceps weakness
Level of evidence: Level 4
Keywords: humerus, olecranon, osteotomy, triceps, anconeus
Introduction
Distal humerus fractures in adults make up 2-7% of all fractures, and often follow high-energy injury.1-5 Non-surgical treatment of these fractures is not routinely indicated as it can be associated with a high risk of stiffness and loss of function.6-9 Adequate open reduction and fixation requires sufficient exposure to visualise the distal humerus including the articular surface.10
The olecranon osteotomy is the workhorse surgical approach to treat AO type C fractures as it provides excellent surgical exposure of the articular surface and unrestricted plating options.10-12 There have been several documented concerns about the osteotomy, which include, from Goda et al., delayed union and non-union (10%), malunion and prominent hardware (25%); from Gofton et al., non-union (13%), heterotopic ossification (30%), infection (9%), reoperation rate (34%); from Kundel et al., non-union (12%), infection (8%), failure of fixation (4%), heterotopic ossification (49%); from Meldrum et al., non-union (3%), infection (3%), implant irritation (22%).13-16 Somerson et al., in a recent paper, reported the olecranon osteotomy to be the only independent predictor for reoperation after fixation of intra-articular distal humerus fractures.17 There has also been some uncertainty as to which method of olecranon osteotomy osteosynthesis is most effective.18-20
Triceps-sparing, -reflecting and -splitting approaches are alternatives, but they provide less access to the intra-articular component.9 An advantage of the triceps-off and triceps-splitting approaches is that retaining the olecranon provides the olecranon, coronoid and radial head as a three-dimensional template to restore humeral articular fragments.21-23
The TOFS approach is not the only triceps-off approach that uses a tendon-to-tendon repair.2428 Others include the Campbell triceps-splitting approach (Figures 1a and b), van Gorder V-to-Y plasty (Figures 1c and d), Newcastle approach to the elbow, and the Shahane and Stanley triceps split and snip. Our approach is unique because it uses an 'h'-shaped transection of the triceps tendon (Figure 1e) that allows the triceps, triceps fascia, anconeus and anconeus fascia to be reflected in continuity, enough to expose the distal humerus articular surface.
Triceps-off approaches provide adequate access and visualisation of distal humerus intra-articular fractures, without compromising vascular supply to anconeus muscle and without the complications associated with olecranon osteotomy.22,23,29-33 The triceps-off approach has been shown to be extensive enough to address most intra-articular distal humerus fractures.23 Tendon-to-tendon repair has been shown to have better healing rates and strength when compared to a tendon-to-bone repair.34,35
Triceps-splitting (Campbell's) approach which involves splitting the triceps aponeurosis and the deep medial head of triceps in the midline has been implicated in postoperative triceps weakness especially when the closure technique uses the V-Y lengthening technique.25,36,37
The Bryan-Morrey triceps-reflecting approach entails lifting the triceps tendon, forearm fascia and periosteum as a single unit from medial to lateral by sharp dissection from the proximal ulna (Figures 1f and g) and is associated with the risk of triceps tendon avulsion and triceps insufficiency.31,38 The triceps attachment has to be protected for at least six weeks postoperatively by avoiding active elbow extension against resistance.30,39
The triceps-reflecting anconeus pedicle (TRAP) approach described by O'Driscoll (Figures 1h and i) is a combination of the modified Kocher and Bryan-Morrey approaches; it claims to preserve the innervation of anconeus muscle and preserves the ligaments at the posterolateral side of elbow.21 It relies on the reattachment of the triceps tendon through drill holes and may be at risk of triceps tendon avulsion from the weakened reattachment as postulated by McKee et al.37,40,41 The transosseous cruciate repair is not an anatomic repair technique and it has been shown in biomechanical studies to have significantly more repair site motion when cyclically loaded.42,43 Clinical data also report re-tear rates of up to 21% after primary repair of the triceps tendon with the use of transosseous tunnels.42,44 The cortical holes used in this technique can also result in a stress riser increasing the risk of fracture.45-47
Studies have suggested that with any triceps-splitting or -reflecting approach there remains the potential of triceps muscle weakness from direct muscle injury, failed tendon reattachment and injury to intramuscular nerves.23,25,41 The TOFS approach is therefore not excluded from this postulation. To the authors' knowledge this is the only study to perform a postoperative ultrasound assessment study of the triceps tendon.
The TOFS approach has been used at our institution for several years, and named as 'the triceps-off, transfascial sleeve approach' (TOFS). It has not been formally described with published outcomes. This study was conducted to describe the surgical technique, functional outcomes and triceps tendon integrity.
Methods
This was an ambispective cohort study of all the patients treated for distal humerus fractures, using a TOFS approach between March 2016 and January 2019 at a tertiary teaching hospital in South Africa. The following were considered to have potentially confounding factors and were therefore excluded: bilateral elbow injuries due to the risk that they will distort triceps strength measurements as triceps strength is quantified as a comparison of the contralateral side (one patient); open fracture, a prognostic factor in itself, as it can alter management and has been shown to have a significant impact on functional outcomes (five); patients with any neural deficiency incurred prior to surgery due to the risk that the deficiency might confuse our findings (two).15,20,48,49 We believe the only contraindication to the TOFS approach are capitellar and trochlear shear fractures. A retrospective review of our prospectively kept surgical database to identify all patients undergoing this approach was performed. Patients' hospital records, surgical notes and X-rays were reviewed. All patients were invited for an elbow sonographic assessment and triceps strength assessment. The study was performed after institutional ethics approval.
A total of 18 patients underwent this surgical approach, with eight being excluded due to the abovementioned exclusion criteria, leaving a final cohort of ten patients. The mean follow-up was 11 months (range 6-19) and nine were females. The mean age was 36.7 ± 14.9 years (range 19-68). Fractures were classified as type C1 (4), C2 (5) and C3 (1) according to the AO classification system. Surgery was either performed by the senior consultant or by a senior registrar under the former's direct supervision. Two patients were operated on their right (in these cases dominant) side and eight patients were operated on their left (in these cases non-dominant) side.
Clinical evaluation and outcome measures
Active elbow range of motion and active flexion-extension arc were measured on the affected and unaffected elbow using a goniometer. For strength testing, the elbow angles used for triceps muscle strength testing were those described by McKee et al.40 Triceps strength was calculated with the aid of a luggage scale measuring against gravity; with the upper arm perpendicular to the floor and forearm in neutral rotation, the readings were taken with the elbow at 45°, 90° and 120° of flexion. The patients had the measuring scale suspended from a strap that was held firmly with a clenched fist (Figures 2a and b). The reading was described as a ratio of the uninjured side. The patients were given two practice attempts to ensure that the patient maintains the correct positions throughout the examination. This sometimes required a guiding hand to ensure the patient fully understood what was required of them during the process prior to the actual strength test.
Radiographic analysis
Preoperative and postoperative plain anteroposterior and lateral radiographs were reviewed by two independent observers (orthopaedic surgeons). We used the same criteria as that of Verma et al. to assess fracture union; fracture union was defined as the presence of bridging callus or the absence of a fracture line on three of four cortices seen on the anteroposterior and lateral radiographs.1 We used criteria similar to Coles et al. to assess intra-articular gap or step-off, an articular gap and/or step of < 2 mm was considered a good reduction, and we expanded on the criteria by including the following: an intra-articular gap and/or step > 2 mm but < 4 mm was considered as fair, and > 4 mm was considered poor.50 X-rays were performed at the six-week and three-month follow-up and thereafter three monthly until union.
Sonographic evaluation
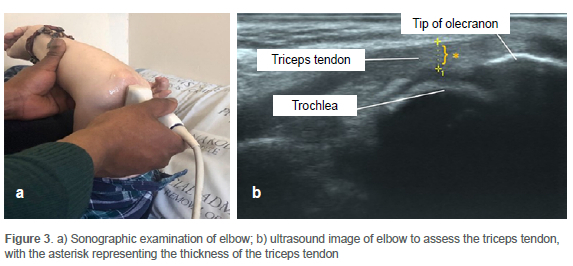
Ultrasonography of the triceps tendon was performed on the operated and unaffected side by an upper limb surgeon with over 15 years of ultrasound experience. The triceps tendon was first measured statically with the elbow at 90° of flexion. The thickness of the tendon was measured 1 cm proximal to insertion triceps and was compared to the opposite side (Figure 3). It was also examined dynamically to confirm tendon integrity.
DASH questionnaire
The disability of the arm, shoulder and hand (DASH) questionnaire was used to measure clinical outcomes. Normal and pain-free function scores as 0 and complete impairment scores 100.40
Surgical technique
All patients were positioned in a lateral position with the arm hanging over a bolster to allow elbow-free motion and traction possible to assist in reduction and fracture exposure. A pneumatic tourniquet was used in all cases.
A lazy-S incision is made beginning on the medial aspect of the arm 15 cm above the olecranon tip to allow adequate exposure of the fracture and the ulna nerve, followed by a gentle curve over the olecranon, then extending 5 cm distal and radial to the olecranon (Figure 4a). The ulnar nerve is identified, released and protected. Once the ulnar nerve has been protected, the medial border of the medial head of triceps is followed distally to the triceps tendon. A transverse full-thickness incision is made across the triceps tendon about 5-10 mm from its insertion into the olecranon tip. This transverse incision ends abruptly after about 2 cm when the incision is continued longitudinally and distally between the lateral aspect of the olecranon/proximal ulna and the anconeus muscle. The goal is a continuous sleeve of triceps, triceps fascia, anconeus and anconeus fascia (Figure 4b). The anconeus fascia is released sharply off the bone for approximately 5 cm to facilitate easy reflection. The triceps tendon and muscle are reflected subperiosteally and laterally off the humerus and retracted with a Hohmann's retractor (Figure 4c), which also aids to displace and protect the radial nerve.

This approach is better suited for orthogonal plating (Figure 4d). It can be difficult to get enough retraction of the triceps mass to expose the lateral aspect for a true lateral plate (parallel plating technique). The intercondylar split can be fixed using interfragmentary screws inserted from lateral to medial.
The triceps tendon is repaired anatomically using no. 1 Vicryl suture.
Postoperative care and rehabilitation
It is the senior author's preference to apply a modified Robert Jones dressing for the first 48 hours and to protect the arm in a sling, while mobilising as pain allows. Rehabilitation of the elbows was started as the pain and swelling decreased. No prophylactic therapy was given to prevent heterotopic ossification. The patients were seen by a physiotherapist prior to discharge and advised against weight bearing and active movements against resistance or gravity for a period of six weeks after surgery. The patients were prescribed a minimum of six weeks of outpatient physiotherapy. A wound inspection and removal of sutures was performed at two weeks.
Statistical analysis
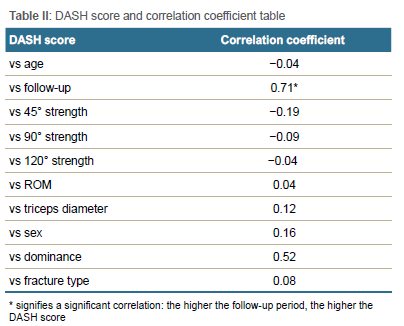
The DASH scores were correlated with the scale values of age, follow-up period, triceps strength (at 45°, 90° and 120° of extension), triceps diameter and range of motion. Two-tailed Pearson's correlation coefficient was calculated for the above comparisons. Further correlation of the DASH scores were performed with categorical values of sex, fracture type, and the injured side (dominance vs non-dominance). Kendall's correlation coefficient was calculated for the above comparisons. The condition for statistical significance was set at p < 0.05. All the statistical analyses were performed in IBM SPSS v.26 (IBM Co., Armonk, NY, USA).
Results
Table I summarises the demographic data and clinical outcome of the study population.
The mean flexion-extension range of motion was 114.7 ± 25.1° (range 80-150), while on the unaffected side the mean was 136° (range 120-150) with a 16% reduction in mean flexion-extension arc relative to the unaffected side. Seven of the ten patients achieved a functional range of motion of 100° as defined by Morrey et al.51
Strength testing revealed the mean percentage of the triceps strength when compared to the opposite side was 66% at 45° of flexion, 70% at 90° and 86% at 120° of elbow flexion. Eight of the ten patients had been injured on the non-dominant arm. Assuming that the non-dominant arm is the weaker arm, we split the group of patients into dominant and non-dominant groups, with the mean triceps strength of the two patients in the dominant group as follows: at 45°, 72%; at 90°, 75%; and at 120°, 99%. In the non-dominant group, consisting of eight patients: at 45°, 64%; at 90°, 70%; and at 120°, 83%. We also divided the groups according to length of follow-up: the first group was made up of five patients who had been assessed at six months after surgery; the second group consisted of five patients who all had their assessment between 13 and 19 months post surgery. The triceps strength was higher in the first group. Mean triceps strength was as follows: first group at 45°, 73%; at 90°, 74%; and at 120°, 82%. The mean triceps strength in the second group was as follows: at 45°, 59%; at 90°, 68%; and at 120°, 90%.
Concerning triceps tendon integrity, the mean triceps diameter on the affected side was 7 mm (range 4-12) and on the unaffected side 8 mm (range 6-13), with a mean of 12% decrease in diameter relative to the contralateral triceps tendon, and the mean difference in size was 1 mm (range 0-3). All triceps tendons were intact, and no gaping was observed.
The mean DASH score was 15.7 ± 8.9 indicating mild residual impairment (range 5-31). The DASH score had a strong positive correlation (r = 0.71; p < 0.05) with the follow-up period. The correlation coefficient between the DASH score and arm dominance was 0.52 (p > 0.05). With all the other factors, the DASH score had very low and insignificant correlations (Table II). Even though certain patients exhibited a higher DASH score at higher follow-ups, their range of motion and joint strength was not significantly different from patients with a low DASH score.
Radiographic analysis
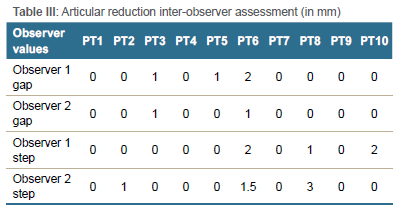
At the time of the six-month follow-up all patients had achieved fracture union and there had been no loss of fracture reduction (Figures 5a-d). The ICC value of 0.66 between the two observers suggests good inter-rater reliability (Table III).

Revision surgery and complications
One of the patients had revision surgery for removal of an infected implant at 11 months post fixation. The diagnosis was made based on a draining wound and confirmed by three positive Staphylococcus aureus culture samples. She was treated with a six-week course of antibiotic therapy (two weeks IV cloxacillin, four weeks oral flucloxacillin). The fracture had united, and the triceps was intact at the time of revision (Figures 5e -j).This patient was excluded from the results of the study due to deep surgical site infection. No other complications were documented. There were no tendon ruptures, loss of reduction and no ulnar nerve complications.
Discussion
McKee et al. retrospectively reported comparable functional outcomes between olecranon osteotomy and triceps-splitting approaches in 26 patients with AO C-type fractures, who were followed up over a mean period of 37 months (range 18-75). The mean range of motion was 108° (range 55-140) and the DASH score was 20 (range 0-50)40 Our results show a similar range of motion of 114.7 ± 25.1 degrees (range 80-150) and a better mean DASH score of 15.7 ± 8.9. Hallgren reported results comparable to our study with functional outcomes in patients with AO C-type fractures treated by means of a triceps-splitting approach. The mean follow-up time was 41 months (range 12-115), the mean DASH score was 24 and the mean ROM was 103° (range 40-150).52 In our study there is a significant correlation between the DASH score and the follow-up time; this finding has to be seen in the correct context which is that the mean DASH score in the long follow-up group was still less than 52 indicating mild residual impairment.40,53 This can be confirmed by observations of acceptable strength and range of motion levels observed for all the patients included in this study. Furthermore, since we are not reporting DASH scores for the same individual for different instances of follow-up, we cannot predict if the reported DASH score was better or worse for patients examined at a longer duration of follow-up. This was a limitation of the current study.
Our patients showed residual triceps weakness. We documented weaker triceps strength at 45° and 90° of elbow flexion compared to the unaffected side, with a mean reduction of 34% and 30% respectively. Triceps strength at 120° flexion showed a 14% reduction as compared to the contralateral side as seen in other studies. McKee et al. do not explain the reason for assessing triceps strength at three different points of elbow flexion.40 Their study reported mean triceps extension strength compared to the unaffected side as follows: at 45°, 76%; at 90°, 74%; and at 120°, 75% of normal, while Hallgren reported a mean triceps strength of 85% of normal in the triceps-splitting group.52 Triceps weakness in our study is a concern but the observations correlate with the current literature.
Transolecranon osteotomy provides excellent exposure of the joint surface; however, osteotomy-related complications are high.9,12,17,31 Gainor et al. reported a 30% osteotomy nonunion rate in ten patients treated for distal humerus fractures with a transolecranon osteotomy, followed up at 24 months.54 Comparative level 1 or 2 studies have not shown superior outcome with any of the approaches.6,55 A systematic review of 38 studies found comparable functional outcomes and complication rates between olecranon osteotomy, triceps-reflecting and triceps-splitting approaches.55
A comparative retrospective study of 43 patients, 16 treated with the paratricipital (triceps-splitting) approach and 27 with olecranon osteotomy found no difference in outcomes and complications among the two groups. The difference between the mean quick DASH score for both groups was not statistically significant. Two patients from the osteotomy group had delayed union.56 However, Elmadag et al. found olecranon osteotomy to have superior functional results over the triceps-splitting approach in 54 patients with intra-articular distal humerus fractures. Fifty-four per cent were treated through transolecranon osteotomy and had better range of motion at final 38 months follow-up. The triceps-splitting approach they describe is different from the TOFS approach as it involves lifting the triceps muscle from its attachment site in a 'V' form, with the fascia loosened proximally, followed by splitting the muscular portion to expose the condyles. They repaired the muscle and tendon with 1.0 absorbable suture. The rate of complications between this triceps-splitting and the olecranon osteotomy group was similar with 50% occurring in the olecranon osteotomy group and 40.6% in the triceps-splitting group. Two patients had osteotomy site non-union and underwent revision surgery with bone graft. Patients who underwent the triceps-splitting approach were immobilised for three weeks compared to two weeks in the osteotomy group. They did not report any tendon ruptures.11 One of the limitations of the Elmadag et al. paper is that they did not perform any objective functional tests, neither triceps strength nor imaging assessment of the triceps tendon. Our patients were immobilised for only 48 hours in a sling after the operation. All of our patients underwent an ultrasound assessment of the triceps. All tendons were found to be intact. Klauser et al. emphasises the reliability of ultrasound as a means of assessing triceps tendon integrity.57
Although the TOFS approach allows orthogonal plating without interfering with joint and anconeus muscle blood supply, this should not cause undue discrimination when compared to parallel plating, as neither has been found to be clinically superior to the other.7 The results of the radiographic analysis suggest that the TOFS approach facilitates accurate reduction and a stable internal fixation of the distal humerus articular joint surface.
A prospective randomised clinical study by Shin et al. compared parallel to orthogonal plating in closed intra-articular distal humeral fractures. They reported no significant differences in outcome between the two groups at a minimum follow-up time of two years. However, two patients had fracture non-unions (one with implant loosening) in the orthogonal group compared to none in the parallel group.7 The TOFS approach, similar to other triceps-off approaches, has been shown to be extensive enough to address most intra-articular distal humerus fractures. We, however, recommend that the TOFS approach not be used for distal humerus fractures that have a coronal split.21-23
Heterotopic ossification (HO) is common following surgery for elbow trauma, with incidence having been reported to be as high as 30-37%.58-62 It i s not clear how much the surgical approach influences the formation of new ectopic bone after elbow surgery. It has been suggested that patients who undergo an olecranon osteotomy are at greater risk of HO because it causes further disruption of the intra-articular continuity of the elbow joint compared to a triceps-sparing approach.39,63 The evidence supports the prophylactic use of non-steroidal anti-inflammatories drugs (NSAIDs) following total hip arthroplasty to reduce HO formation.64 There is less evidence to support their use following elbow surgery.64,65 A recent cohort study investigated the efficacy of NSAIDs to reduce the incidence of HO following surgery for elbow trauma and found no benefit.66 NSAID use also potentially increases the potential risk of fracture non-union.67 There is also little evidence to support the use of radiation therapy (RT) to prevent HO formation, and the associated potential risk of fracture non-union remains a concern.68,69 Our study did not prescribe to the use of NSAIDs or radiation therapy as prophylaxis to prevent HO formation.
The variability of reported outcome measures and reporting inconsistencies in the literature with respect to fracture severity and patient factors are elements that make it difficult to compare the different techniques used to manage distal humerus fractures.6,55,70 The outcome measures we used to assess functional outcomes following surgery for elbow trauma are of the prescribed standard, and we also excluded some of the potential confounding factors (open fractures, nerve injuries, bilateral humerus fractures) to allow for the effects of the approach to be better characterised.71
TOFS is a safe and straightforward surgical approach to the distal humerus. Our findings show that the TOFS approach is extensile enough to treat AO type C distal humerus fractures. The patients treated with this approach recover to the level of a mild residual physical impairment and acceptable range of motion comparable to the literature. Excellent union rates and reduction of fractures is possible with this approach. Residual weakness of the triceps is a concern despite the good healing rates of the tendon documented on ultrasound.
We acknowledge that our results are limited by the retrospective nature of this study, small sample size, short duration of follow-up and failure of our patients to adhere to strict rehabilitation. Plain radiographic measurement of articular reduction is not as good as CT scan to assess joint congruity after reduction but to the authors' knowledge there are no studies that have used this method. Financial constraints prevented the use of CT scans for our study. The exact time of union could not be established due to the fact that patients did not attend all routine follow-up visits. This might be due to socioeconomic challenges facing our population. Another limitation of the study was that the DASH questionnaire was only performed once for each patient, and we did not perform a change in DASH which would have allowed us to compare each patient's progression over time.
This study describes the surgical approach and clinical, sonographic and radiological outcomes of this procedure despite described limitations ensuring external validity.
There is a need for a prospective, comparative multicentric study to compare the TOFS approach to other surgical approaches using a standardised method of assessing functional outcomes following the treatment of distal intra-articular humerus fractures in a larger group of patients with adequate representation of each fracture subgroup.
Conclusion
The TOFS approach is effective in treating unilateral, closed fractures where there is no nerve injury where orthogonal plating is undertaken. Those patients were excluded and this plating configuration was used.
Acknowledgement
We are grateful to Ms Stacey Black for assisting us with the illustrations.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010. Prior to commencement of the study, ethical approval was obtained from the following ethical review board: Human Research Ethics Committee, HREC REF: 853/2017. Informed consent was obtained from all individual participants included in the study. All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
WBN: data capture, design of testing set-up, manuscript preparation, first draft
preparation, manuscript revision
PAR: manuscript revision
RD: data analysis
SM: first draft preparation
SR: study design, design of testing set-up
MS: study conceptualisation, design of testing set-up
ORCID
Nkomo WB https://orcid.org/0000-0003-4173-8792
Rachuene PA https://orcid.org/0000-0003-4045-5301
Dey R https://orcid.org/0000-0002-3616-1995
References
1. Verma R, Choudhari R, Bohra A, Sharma S. Management of supracondylar/intercondylar distal humerus fractures using triceps-reflecting anconeus pedicle approach. J Orthop Traumatol Rehabil. 2019;11(1):53. https://doi.org/10.4103/jotr.jotr_19_19 [ Links ]
2. Zalavras CG, Papasoulis E. Intra-articular fractures of the distal humerus-a review of the current practice. Int Orthop. 2018;42(11):2653-62. https://doi.org/10.1007/s00264-017-3719-4 [ Links ]
3. Amir S, Jannis S, Daniel R. Distal humerus fractures: a review of current therapy concepts. Curr Rev Musculoskelet Med. 2016;9(2):199-206. https://doi.org/10.1007/s12178-016-9341-z [ Links ]
4. Robinson CM, Hill RMF, Jacobs N, et al. Adult distal humeral metaphyseal fractures: epidemiology and and results of treatment. J Orthop Trauma. 2003;17(1):38-47. [ Links ]
5. Lauder A, Richard MJ. Management of distal humerus fractures. Eur J Orthop Surg Traumatol. 2020;30(5):745-62. https://doi.org/10.1007/s00590-020-02626-1 [ Links ]
6. Ljungquist KL, Beran MC, Awan H. Effects of surgical approach on functional outcomes of open reduction and internal fixation of intra-articular distal humeral fractures: a systematic review. J Shoulder Elb Surg. 2020;21(1):126-35. https://doi.org/10.1016/jjse.2011.06.020 [ Links ]
7. Shin SJ, Sohn HS, Do NH. A clinical comparison of two different double plating methods for intraarticular distal humerus fractures. J Shoulder Elb Surg. 2010;19(1):2-9. https://doi.org/10.1016/j.jse.2009.05.003 [ Links ]
8. Riseborough EJ, Radin EL. Intercondylar T fractures of the humerus in the adult. A comparison of operative and non-operative treatment in twenty-nine cases. J Bone Joint Surg Am. 1969;51(1):130-41. [ Links ]
9. Pollock JW, Faber KJ, Athwal GS. Distal humerus fractures. Orthop Clin North Am. 2008;39(2):187-200. https://doi.org/10.1016/j.ocl.2007.12.002 [ Links ]
10. Wilkinson JM, Stanley D. Posterior surgical approaches to the elbow: A comparative anatomic study. J Shoulder Elb Surg. 2001;10(4):380-82. https://doi.org/10.1067/mse.2001.116517 [ Links ]
11. Elmadag M, Erdil M, Bilsel K, et al. The olecranon osteotomy provides better outcome than the triceps-lifting approach for the treatment of distal humerus fractures. Eur J Orthop Surg Traumatol. 2014;24(1):43-50. https://doi.org/10.1007/s00590-012-1149-y [ Links ]
12. Pradhan DCS, Gupta DT, Mohapatra DN, et al. Evaluation of surgical treatment of inter-condylar humerus fracture with olecranon osteotomy approach. Int J Orthop Sci. 2018;4(4):481-85. https://doi.org/10.22271/ortho.2018.v4.i4e.50 [ Links ]
13. Goda MK, Radwan YA, Mansour AM, et al. Triceps anconeus sparring approach versus olecranon osteotomy in treatment of intercondylar fracture humerus. Med J Cairo Univ. 2018;86(5):2775-80. [ Links ]
14. Gofton WT, MacDermid JC, Patterson SD, et al. Functional outcome of AO type C distal humeral fractures. J Hand Surg Am. 2003;28(2):294-308. https://doi.org/10.1053/jhsu.2003.50038 [ Links ]
15. Kundel K, Braun W, Wieberneit J, Rüter A. Intraarticular distal humerus fractures: Factors affecting functional outcome. Clin Orthop Relat Res. 1996;(332):200-208. https://doi.org/10.1097/00003086-199611000-00027 [ Links ]
16. Meldrum A, Kwong C, Archibold K, et al. Olecranon osteotomy implant removal rates and associated complications. J Orthop Trauma. 2021;35(5):265-70. https://doi.org/10.1097/BOT.0000000000001979 [ Links ]
17. Somerson JS, Morrey ME, Sanchez-Sotelo J, Morrey BF. Predictors of reoperation after internal fixation of intra-articular distal humerus fractures. Shoulder Elb. 2022;14(1):76-83. https://doi.org/10.1177/1758573219895972 [ Links ]
18. Duckworth AD, Clement ND, White TO, et al. Plate versus tension-band wire fixation for olecranon fractures. J Bone Jt Surg Am. 2017;99(15):1261-73. https://doi.org/10.2106/JBJS.16.00773 [ Links ]
19. Nijs S, Graeler H, Bellemans J. Fixing simple olecranon fractures with the olecranon osteotomy nail (OleON). Oper Orthop Traumatol. 2011;23(5):438-45. https://doi.org/10.1007/s00064-011-0112-0 [ Links ]
20. Woods BI, Rosario BL, Siska PA, et al. Determining the efficacy of screw and washer fixation as a method for securing olecranon osteotomies used in the surgical management of intraarticular distal humerus fractures. J Orthop Trauma. 2015;29(1):44-49. https://doi.org/10.1097/BOT.0000000000000131 [ Links ]
21. O'Driscoll SW. The triceps-reflecting anconeus pedicle (TRAP) approach for distal humeral fractures and nonunions. Orthop Clin North Am. 2000;31(1):91-101. https://doi.org/10.1016/S0030-5898(05)70130-9 [ Links ]
22. Chou YC, Hsu YH, Yu YH, Wu CC. Triceps-reflecting anconeus pedicle approach with double precontoured locking plate fixation is efficient in the treatment of orthopaedic trauma association type C distal humerus fracture. Injury. 2016;47(10):2240-46. https://doi.org/10.1016/j.injury.2016.06.036 [ Links ]
23. Ozer H, Solak S, Turanli S, et al. Intercondylar fractures of the distal humerus treated with the triceps-reflecting anconeus pedicle approach. Arch Orthop Trauma Surg. 2005;125(7):469-74. https://doi.org/10.1007/s00402-005-0026-0 [ Links ]
24. Campbell WC. Incision for exposure of the elbow joint. Am J Surg. 1932;15(1):65-67. https://doi.org/10.1016/S0002-9610(32)90997-0 [ Links ]
25. Van Gorder G. Surgical approach in supracondylar 'T' fractures of the humerus. J Bone Joint Surg Am. 1940;22(2):278-92. [ Links ]
26. Amirfeyz R, Clark D, Quick T, Blewitt N. Newcastle approach to the elbow, a cadaveric study. Arch Orthop Trauma Surg. 2011;131(6):747-51. https://doi.org/10.1007/s00402-010-1206-0 [ Links ]
27. Shahane SA, Stanley D. A posterior approach to the elbow joint. J Bone Joint Surg Br. 1999;81-B(6):1020-22. https://doi.org/10.1302/0301-620x.81b6.0811020 [ Links ]
28. Poon PC, Foliaki S, Young SW, et al. Triceps Split and Snip approach to the elbow: surgical technique and biomechanical evaluation. ANZ J Surg. 2013;83(1):774-8. https://doi.org/10.1111/ans.12131 [ Links ]
29. Azboy i, Bulut M, Ancar C, et al. The comparison of triceps-reflecting anconeus pedicle and olecranon osteotomy approaches in the treatment of intercondylar fractures of the humerus. Ulus Travma ve Acil Cerrahi Derg. 2016;22(1):58-65. https://doi.org/10.5505/tjtes.2015.42948 [ Links ]
30. Zhang C, Zhong B, Luo CF. Comparing approaches to expose type C fractures of the distal humerus for ORIF in elderly patients: Six years clinical experience with both the triceps-sparing approach and olecranon osteotomy. Arch Orthop Trauma Surg. 2014;134(6):803-11. https://doi.org/10.1007/s00402-014-1983-y [ Links ]
31. Fernández-Valencia JA, Muñoz-Mahamud E, Ballesteros JR, Prat S. Treatment of AO type C fractures of the distal part of the humerus through the Bryan-Morrey triceps-sparing approach. ISRN Orthop. 2013;2013:1-6. https://doi.org/10.1155/2013/525326 [ Links ]
32. Deakin DE, Deshmukh SC. The triceps-flexor carpi ulnaris (TRIFCU) approach to the elbow. Ann R Coll Surg Engl. 2010;92(3):240-42. https://doi.org/10.1308/003588410X12628812458536 [ Links ]
33. Peach C, Stanley D. Surgical approaches to the elbow. Orthop Trauma. 2012;26(5):297-302. https://doi.org/10.1016/j.mporth.2012.09.008 [ Links ]
34. Clark J, Obopilwe E, Rizzi A, Komatsu D. Distal Triceps knotless anatomic footprint repair is superior to transosseous cruciate repair: a biomechanical comparison. J Arthrosc Relat Surg. 2014;30(10):254-60. https://doi.org/10.1016/j.arthro.2014.07.005 [ Links ]
35. Scheiderer B, Lacheta L, Imhoff AB, Siebenlist S. V-shaped double-row distal triceps tendon repair: A novel technique using unicortical button fixation. Eur J Med Res. 2017;22(1):9. https://doi.org/10.1186/s40001-017-0250-4 [ Links ]
36. MacAusland WR. Ankylosis of the elbow: With report of four cases treated by arthroplasty. J Am Med Assoc. 1915;LXIV(4):312-18. https://doi.org/10.1001/jama.1915.02570300026009 [ Links ]
37. Kasser JR, Richards KPT, Millis MMD. The triceps-dividing approach to open reduction of complex distal humeral fractures in adolescents: a Cybex evaluation of triceps function and motion. J Pediatr Orthop. 1990;10(1):93-96. [ Links ]
38. Inglis AE, Pellicci PM. Total elbow replacement. J Bone Jt Surg Am. 1980;62(8):1252-58. https://pubmed.ncbi.nlm.nih.gov/7440604/ [ Links ]
39. Chen G, Liao Q, Luo W, et al. Triceps-sparing versus olecranon osteotomy for ORIF: Analysis of 67 cases of intercondylar fractures of the distal humerus. Injury. 2011;42(4):366-70. https://doi.org/10.1016/j.injury.2010.09.004 [ Links ]
40. McKee MD, Wilson TL, Winston L, et al. Functional outcome following surgical treatment of intra-articular distal humeral fractures through a posterior approach. J Bone Jt Surg Am. 2000;82(12):1701-707. https://doi.org/10.2106/00004623-200012000-00003 [ Links ]
41. Bryan RS, Morrey BF. Extensive posterior exposure of the elbow. A triceps-sparing approach. Clin Orthop Relat Res. 1982;166:188-92. https://doi.org/10.1097/00003086-198206000-00033 [ Links ]
42. Scheiderer B, Imhoff FB, Morikawa D, et al. The V-shaped distal triceps tendon repair: a comparative biomechanical analysis. Am J Sports Med. 2018;46(8):1952-58. https://doi.org/10.1177/0363546518771359 [ Links ]
43. Yeh PC, Stephens KT, Solovyova O, et al. The distal triceps tendon footprint and a biomechanical analysis of 3 repair techniques. Am J Sports Med. 2010;38(5):1025-33. https://doi.org/10.1177/0363546509358319 [ Links ]
44. Van Riet R, Morrey B, Ho E, O'Driscoll S. Surgical treatment of distal triceps ruptures. J Bone Jt Surg. 2003;85(10):1961-67. https://doi.org/10.2106/00004623-200310000-00015 [ Links ]
45. Tan H, Wang D, Lebaschi AH, et al. Comparison of bone tunnel and cortical surface tendon-to-bone healing in a rabbit model of biceps tenodesis. J Bone Jt Surg Am. 2018;100(6):479-86. https://doi.org/10.2106/JBJS.17.00797 [ Links ]
46. Sears BW, Spencer EE, Getz CL. Humeral fracture following subpectoral biceps tenodesis in 2 active, healthy patients. J Shoulder Elbow Surg. 2011 ;20(6):e7-11. https://doi.org/10.1016/j.jse.2011.02.020 [ Links ]
47. Dein EJ, Huri G, Gordon JC, McFarland EG. A humerus fracture in a baseball pitcher after biceps tenodesis. Am J Sports Med. 2014;42(4):877-79. https://doi.org/10.1177/0363546513519218 [ Links ]
48. Cho E, Weber MB, Opel D, et al. Complications and functional outcomes after transolecranon distal humerus fracture. J Shoulder Elb Surg. 2021;30(3):479-86. https://doi.org/10.1016/j.jse.2020.07.012 [ Links ]
49. Ahmed AF, Parambathkandi AM, Kong WJG, et al. The role of ulnar nerve subcutaneous anterior transposition during open reduction and internal fixation of distal humerus fractures: a retrospective cohort study. Int Orthop. 2020;44(12):2701-708. https://doi.org/10.1007/s00264-020-04745-0 [ Links ]
50. Coles CP, Barei DP, Nork SE, et al. The olecranon osteotomy: a six-year experience in the treatment of intraarticular fractures of the distal humerus. J Orthop Trauma. 2006;20(3):163-70. https://doi.org/10.1097/00005131-200603000-00002 [ Links ]
51. Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Jt Surg. 1981;63(6):872-77. [ Links ]
52. Hallgren HB. Triceps split: a safe and useful approach for distal humeral fractures. Biomed J Sci Tech Res. 2020;24(5):18617-24. https://doi.org/10.26717/bjstr.2020.24.004115 [ Links ]
53. Williams N. DASH. Occup Med (Lond). 2014;64(1):67-68. https://doi.org/10.1093/occmed/kqt130 [ Links ]
54. Galnor BJ, Moussa F, Schott T. Healing rate of transverse osteotomies of the olecranon used in reconstruction of distal humerus fractures. J South Orthop Assoc. 1995;4(4):263-68. [ Links ]
55. Sharma S, John R, Dhillon MS, Kishore K. Surgical approaches for open reduction and internal fixation of intra-articular distal humerus fractures in adults: A systematic review and meta-analysis. Injury. 2018;49(8):1381-91. https://doi.org/10.1016/jjnjury.2018.06.018 [ Links ]
56. Atif M, Hasan O, Mohib Y, et al. Does surgical approach affect outcome after fixation of intra-articular fractures of distal humerus? Retrospective cohort study from a level-1 trauma centre in a metropolitan city. Ann Med Surg (Lond). 2019;43:48-51. https://doi.org/10.1016/j.amsu.2019.05.012 [ Links ]
57. Klauser AS, Tagliafico A, Allen GM, et al. Clinical indications for musculoskeletal ultrasound: A Delphi-based consensus paper of the European society of musculoskeletal radiology. Eur Radiol. 2012;22(5):1140-48. https://doi.org/10.1007/s00330-011-2356-3 [ Links ]
58. Ilahi OA, Strausser DW, Gabel GT. Post-traumatic heterotopic ossification about the elbow. Orthopedics. 1998;21(3):265-68. https://doi.org/10.3928/0147-7447-19980301-09 [ Links ]
59. Herman ZJ, Edelman DG, Ilyas AM. Heterotopic ossification after elbow fractures. Orthopedics. 2020;44(1):10-16. https://doi.org/10.3928/01477447-20201119-03 [ Links ]
60. Abrams GD, Bellino MJ, Cheung EV. Risk factors for development of heterotopic ossification of the elbow after fracture fixation. J Shoulder Elb Surg. 2012;21(11):1550-54. https://doi.org/10.1016/J.JSE.2012.05.040 [ Links ]
61. Foruria AM, Lawrence TM, Augustin S, et al. Heterotopic ossification after surgery for distal humeral fractures. Bone Jt J. 2014;96B(12):1681-87. https://doi.org/10.1302/0301-620X.96B12.34091 [ Links ]
62. Hong CC, Nashi N, Hey HW, et al. Clinically relevant heterotopic ossification after elbow fracture surgery: A risk factors study. Orthop Traumatol Surg Res. 2015;101(2):209-13. https://doi.org/10.1016/j.otsr.2014.10.021 [ Links ]
63. Cheung EV, Sarkissian EJ. Complications of elbow trauma. Hand Clin. 2015;31(4):683-91. https://doi.org/10.1016/jhcl.2015.06.012 [ Links ]
64. Meyers C, Lisiecki J, Miller S, et al. Heterotopic ossification: a comprehensive review. JBMR Plus. 2019;3(4):e10172. https://doi.org/10.1002/jbm4.10172 [ Links ]
65. Savvidou OD, Zampeli F, Koutsouradis P, et al. Complications of open reduction and internal fixation of distal humerus fractures. EFORT Open Rev. 2018;3(10):558-67. https://doi.org/10.1302/2058-5241.3.180009 [ Links ]
66. Bochat K, Mattin AC, Ricciardo BJ. The efficacy of nonsteroidal anti-inflammatories in the prevention of heterotopic ossification following elbow trauma surgery. JSES Int. 2021;5(4):793-96. https://doi.org/10.1016/j.jseint.2021.04.004 [ Links ]
67. Murnaghan M, Li G, Marsh DR. Nonsteroidal anti-inflammatory drug-induced fracture nonunion: An inhibition of angiogenesis? J Bone Joint Surg Am. 2006;88 Suppl 3:140-47. https://doi.org/10.2106/JBJS.F00454 [ Links ]
68. Hamid N, Ashraf N, Bosse MJ, et al. Radiation therapy for heterotopic ossification prophylaxis acutely after elbow trauma: A prospective randomized study. J Bone Jt Surg Am. 2010;92(11):2032-38. https://doi.org/10.2106/JBJS.L01435 [ Links ]
69. Ploumis A, Belbasis L, Ntzani E, et al. Radiotherapy for prevention of heterotopic ossification of the elbow: A systematic review of the literature. J Shoulder Elb Surg. 2013;22(11):1580-88. https://doi.org/10.1016/jjse.2013.07.045 [ Links ]
70. Chen H, Li D, Zhang J, Xiong X. Comparison of treatments in patients with distal humerus intercondylar fracture: a systematic review and meta-analysis. Ann Med. 2017;49(7):613-25. https://doi.org/10.1080/07853890.2017.1335429 [ Links ]
71. Zarezadeh A, Mamelson K, Thomas WC, et al. Outcomes of distal humerus fractures: What are we measuring? Orthop Traumatol Surg Res. 2018;104(8):1253-58. https://doi.org/10.1016/j.otsr.2018.08.017 [ Links ]
Received: March 2021
Accepted: November 2021
Published: August 2022
* Corresponding author: w.b.nkomo1@gmail.com
Editor: Dr Ajmal Ikram, Stellenbosch University, Cape Town, South Africa
Funding: No external funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.













