Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671Print version ISSN 1994-3032
S. Afr. j. child health vol.8 n.4 Pretoria Nov. 2014
https://doi.org/10.7196/SAJCH.661
RESEARCH
Maternal sociodemographic factors that influence full child immunisation uptake in Nigeria
O D I ChidiebereI; E UchennaII; O S KenechiIII
IMD, MSc, MPH, FRSPH; Pneumococcal Surveillance Project, Child Survival Unit, Medical Research Council UK, Banjul, The Gambia; Department of Paediatrics, Nnamdi Azikiwe University Teaching Hospital, Nnewi, Nigeria
IIMD, FMC Paed; Department of Paediatrics, Enugu State University Teaching Hospital, Parklane, Enugu, Nigeria
IIIMD, FWAC (Paed); Department of Paediatrics, Nnamdi Azikiwe University Teaching Hospital, Nnewi, Nigeria
ABSTRACT
BACKGROUND: With vaccine-preventable disease accounting for many <5-year deaths in most developing countries, it is imperative to determine the factors responsible for poor immunisation coverage in these countries.
OBJECTIVE: To identify maternal sociodemographic factors associated with child immunisation uptake in Nigeria.
METHODS: Data from a nationally representative sample of mothers (aged 15 - 49 years) were obtained from the 2008 Nigeria demographic and health survey. Logistic regressions were used to examine the association between maternal sociodemographic variables and child immunisation uptake.
RESULTS: The overall uptake of full immunisation based on the National Programme on Immunisation schedule was 30.6%. There was wide variation in full immunisation uptake in the different regions in Nigeria, with 51% in the South-West, 46.5% in the South-East, 39.5% in the South-South, 6.4% in the North-West, 11.8% in the North-East and 28.2% in the North-Central. Approximately 40.2% of children surveyed had never received any form of vaccination. The most common reasons given for non-vaccination of these children were lack of information about immunisation, fear of side-effects and the immunisation centres being too far away. It was noted that uptake of vaccines with multiple dosing schedules dropped with each successive dose. Decreased likelihood for full immunisation was seen in mothers <18 years old (odds ratio (OR) 0.53; confidence interval (CI) 0.34 - 0.84) and mothers residing in the northern regions. Increased likelihood for full immunisation was seen in mothers from middle and rich classes (OR 1.26, CI 1.03 - 1.66 and OR 1.69, CI 1.27 - 2.25, respectively), mothers with higher educational level (OR 3.77, CI 1.52 - 9.32), mothers with access to media (OR 1.84, CI 1.21 - 1.68), mothers resident in urban areas (OR 1.36, CI 1.22 - 1.51) and mothers who had institutional deliveries (OR 1.86, CI 1.44 - 2.40).
CONCLUSION: Full immunisation uptake in Nigeria is poor. Cultural disparity in different regions of Nigeria may account for the wide variation in immunisation coverage observed.
According to the World Health Organization (WHO), about half of all <5-year deaths in the world occur in Africa, and over 70% of these deaths occur within the first year of life.[1] Immunisation is no doubt one of the most successful and cost-effective public health interventions in the history of medicine and biomedical research for preventing death in children <5 years old.[2] Immunisation prevents an estimated 2 - 3 million deaths every year from diphtheria, tetanus, pertussis (whooping cough) and measles.[3] According to a WHO report, full immunisation coverage can prevent 1 in 7 child deaths globally.[4] Africa and Asia still lag behind, with the lowest immunisation rates.[5 ] In 2012, an estimated 22.6 million infants worldwide did not receive routine immunisation services, of which more than half live in three countries: India, Indonesia and Nigeria.[3]
Routine immunisation schedules stipulate that infants should be vaccinated at birth, 6, 10 and 14 weeks of age with Bacille de Calmete et Guérin (BCG), oral polio vaccine (OPV) and diphtheria, pertussis and tetanus (DPT). One dose of vitamin A (though not a vaccine) and measles vaccine should be given at 6 and 9 months, respectively.[6]
Nigeria still has one of the lowest immunisation uptake rates in Africa (30% in 2006).[7] Several studies have linked maternal factors such as age, poor education, poor access to health facilities, single parenting, inadequate antenatal care, ethnicity and negative belief in vaccination to low immunisation uptake around the world, but only a few have then investigated the reasons for poor immunisation uptake.[8-11] The objective of the study was to identify the maternal sociodemographic factors that are associated with child immunisation uptake in Nigeria.
Methods
Study area
Nigeria is in West Africa. The 2006 population and housing census puts Nigeria's population at 140 431 790, making it the most populous nation in Africa and 14th in the world.[12] Nigeria comprises 36 states and the Federal Capital Territory, and is divided into six geopolitical regions: North-Central, North-East, North-West, South-East, South-West and South-South. There are 774 constitutionally recognised local governments and approximately 374 identifiable ethnic groups.[13] This survey was conducted in all states, including the Federal Capital Territory, within the six regions of Nigeria.
Study design and subject
This cross-sectional, descriptive and analytical study used data from the 2008 edition of the Demographic and Health Survey (DHS), a nationally representative probability sample. The DHS used a stratified two-stage cluster sampling design consisting of 888 clusters: 286 urban and 602 rural areas. In all, a nationally representative sample of 36 298 households was selected for the 2008 Nigeria DHS. From these households, 34 596 women were eligible for interview (having at least one child under 5 years old), out of which 33 385 were successfully interviewed, yielding a response rate of 96.5%.[14]
Data collection
The detailed survey methodology has been described elsewhere.[14] Information collected included birth history and in-depth demographic and socioeconomic information. History of illnesses, medical care received, immunisations status and anthropometric measurements of the children were also recorded. Immunisation status of children between 0 and 23 months was determined from vaccination cards shown to the DHS interviewer. In the absence of vaccination cards, where possible mothers were asked to recall whether the child had received BCG, OPV, DPT (including the number of doses for each) and measles vaccinations.[14]
Outcome variable
The outcome variable was the number of mothers who fully vaccinated their children in the last 23 months according to the national immunisation schedule in Nigeria. Hepatitis B and yellow fever vaccines were introduced in 2004, but their availability still remains limited in most public and private health facilities across the country.
Predictor variables
- Current maternal age in years was categorised as 15 - 18, 19 - 34 and 35 - 45.
- Educational level was categorised as no education, primary education and secondary education or higher.
- Place of residence was categorised as rural or urban.
- Occupation status was categorised as unemployed, unskilled and skilled.
- Ethnicity was categorised into the main ethnic groups and the minor groups where categorised as others. Categories were Hausa, Ibo, Yoruba, Fulani, Tiv, Kanuri, Ibibio, Ijaw and Other.
- Wealth status was categorised as poor, middle and rich.
- Religion was categorised as Christian, Muslim and other.
- Decision-making autonomy was categorised as yes or no.
- Access to media was categorised as yes or no.
- Number of living children was categorised as 1 - 3, 4 - 6 and ≥7.
- Place of delivery was categorised as institutional (healthcare setting) or home (traditional birth attendant).
- Birth rank of child was categorised as 1st, 2nd, 3rd and ≥4th.
- Sex of the child was categorised as male or female.
- Geopolitical regions of Nigeria were categorised as North-Central, North-West, North-East, South-West, South-East and South-South. Categorisation of study participants into region of residence was based on this geopolitical division.
Statistical analysis
The Predictive Analytics Software statistical package version 19.0 (SPSS Inc., USA) was used for data analysis. The Pearson χ2 test was used to study the differences in proportion between the independent variables and immunisation uptake. Logistic regressions were used to determine the main maternal factors that predicted full immunisation practice in the study subject after confounders were adjusted for. Results were presented using percentages, odds ratios (ORs) and 95% confidence intervals (CIs) where appropriate. Statistical significance was set at p<0.05.
Ethical consideration
The survey was approved by the Macro International Inc. ethics committee, an Opinion Research Corporation Company (ORC Macro) at Calverton, USA, and by the Ministry of Health ethics committee in Nigeria. Consent was also obtained by data collectors from all mothers before data collection was done for the 2008 Nigeria DHS.[14]
Results
Characteristics of study population
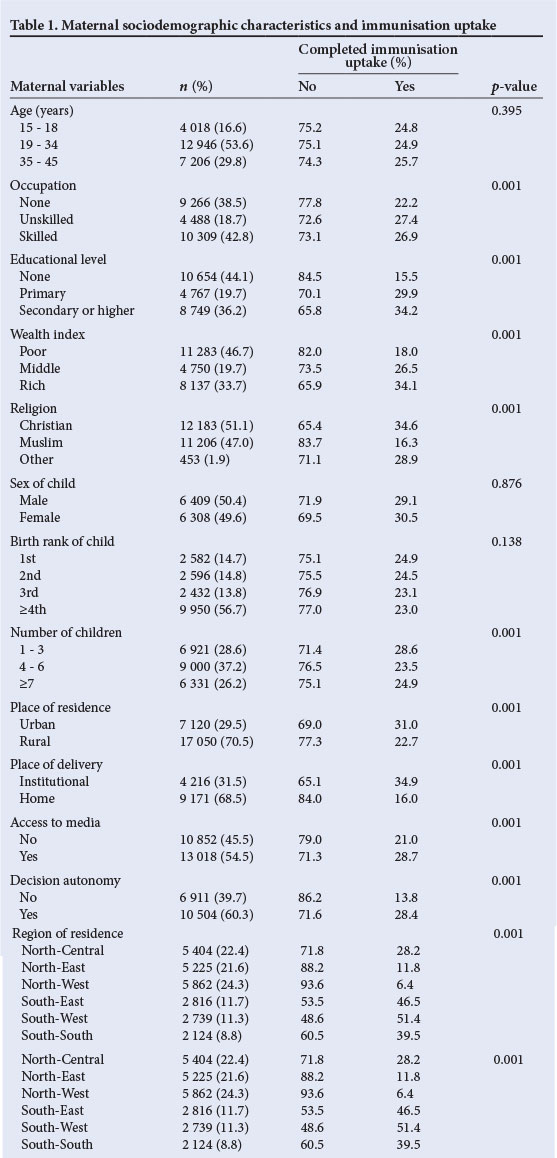
From the 36 298 households identified during the 2008 DHS, 33 385 (96.5%) consented to participate and were successfully interviewed. The majority of the study participants were women between the ages of 19 and 34 years (53.6%) and from the poor wealth class (46.7%) (Table 1). The religion of the participants reflected the two dominant religions in Nigeria, with 51.1% Christian and 47.0% Muslim. Most of the women interviewed were resident in rural areas of the country. Only 31.5% gave birth to their participating child in a health facility. Almost half of those interviewed (54.5%) had access to media and nearly 2/3 (60.3%) had decision autonomy. The majority of the participants had 4 - 6 children, with the index child being commonly ≥4th in birth rank. Sex of the index child was almost equally male (50.4%) and female (49.6%).
Immunisation uptake among children
Full and complete vaccination according to schedule was seen in 30.6% of children surveyed, and 40.0% had never received any form of vaccination. Mothers were least compliant with uptake of vitamin A for their children (37.2%) as part of the immunisation schedule. Dropout rate for OPV and DPT vaccines increased with the dosing schedule, i.e. OPV1, OPV2, OPV3 uptake was 63.3%, 53.6% and 36.0%, respectively, while DPT1, DPT2 and DPT3 uptake was 46.5%, 38.9% and 30.4%, respectively. Reasons given by mothers for refusal to take up and/or complete the vaccination schedule included: lack of information about immunisation schedule (22.4%), fear of side-effects (16.6%), religion forbids vaccination (5.0%), vaccination centres too far away (12.1%), vaccination has no effect (2.0%) and no reason (11.8%).
Maternal sociodemographic factors
Table 1 shows the maternal factors associated with full immunisation uptake among children in the study. Mothers having an occupation (p=0.001), higher educational status (p=0.001), higher wealth class (p=0.001) and being non-Muslim (p=0.001) were significantly associated with higher child immunisation uptake. Having fewer children (p=0.001), urban residence (p=0.001), institutional delivery (p=0.001), access to media (p=0.001), decision-making autonomy (p=0.001) and residence in the southern part of Nigeria (p=0.001) also strongly determined positive immunisation uptake. Within ethnic groups, uptake was lowest among participants from Kanuri (6.2%), Hausa (7.8%), Fulani (14.5%) and Tiv (22.0%), who are mainly from the northern and middle regions of Nigeria, while mothers from the Igala (36.2%), Ijaw (36.8%), Ibibio (42.1%), Ibo (44.5%) and the Yoruba (46.8%) ethnic groups had higher vaccination uptake for their children (Fig. 1).
Final regression model showed that the age, wealth category, educational level, access to media, decision-making autonomy, place and region of residence significantly predicted positive immunisation uptake. Mothers within the 35 - 45 years age bracket were more likely to take up vaccination compared with those in the 15 - 18 (OR 0.53, CI 0.34 - 0.84) and 19 - 34 years age bracket (OR 0.94, CI 0.74 - 1.25). Similarly, mothers in the middle wealth class (OR 1.26, CI 1.03 - 1.66) and those in rich wealth class (OR 1.69, CI 1.27 - 2.25) were more likely to take up vaccination compared with those from the poor wealth class. Not surprisingly, mothers with primary education (OR 1.26, CI 1.03 - 1.66) and those with secondary or higher education (OR 3.77, CI 1.52 - 9.32) were about 1.3 and 3.8 times, respectively, more likely to fully vaccinate compared with those with no education (Table 2).

Furthermore, mothers with access to media (OR 1.84, CI 1.21 - 1.68), those who had institutional deliveries (OR 1.86, CI 1.44 - 2.40) and those resident in urban areas (OR 1.36, CI 1.22 - 1.51) were also more likely to complete vaccination schedules for their children (Table 2). Finally, mothers in the North-East (OR 1.24, CI 1.06 - 1.43) and South-West (OR 1.57, CI 1.23 - 2.01) were about 1.2 and 1.6 times, respectively, more likely to vaccinate their children fully, while those in the South-East (OR 0.57, CI 0.37 - 0.89) and South-South (OR 0.93, CI 0.73 - 1.57) regions were 0.6 and 0.9 times, respectively, less likely to vaccinate their children fully when compared with mothers from the North-Central region of Nigeria (Table 2).
Discussion
Full immunisation uptake in children according to the national immunisation schedule in Nigeria is low (30.6%) compared with the uptake rate in other developing countries. [15] This is disturbing and unacceptable in a country where infant mortality rate is among the highest in the world, and 40% of these deaths are attributed to vaccine-preventable diseases.[16, 17]
There is a high disparity in the likelihood of fully vaccinating a child in the different regions of Nigeria. The northern part of Nigeria was seen to have a lower full immunisation uptake rate when compared with the southern part. The reason for this trend may be related to the fact that mothers from the northern part of Nigeria are generally less educated and economically empowered than their southern counterparts.[18] Furthermore, the northern parts of the country are predominantly populated by Muslims, some of whom have faith-inspired concerns against vaccination programmes. In recent years, the north of Nigeria has also been an insurgence and terrorism frontline, which critically hampers childhood vaccination programmes. Such waves of violence and conflict often engender demographic dislocation, which detracts from proper planning of vaccination programmes.
This study also highlighted the influence of the place of residence on the likelihood of fully vaccinating a child. Mothers who reside in urban area were more likely to vaccinate their children fully compared with those in rural areas. With a higher proportion of Nigerians living in rural areas,[19] this is very disturbing. The reasons for the differences in immunisation uptake seen between rural and urban areas are readily obvious. Due to the higher number of health institutions and centres in urban locations, immunisation services are more easily accessible to mothers. Poor access to and limited healthcare facilities in rural and riverine communities or remote, sandy and mountainous rural settlements in northern Nigeria could also contribute to lower immunisation uptake.
Higher maternal wealth index and education positively influence immunisation uptake, as confirmed in other studies.[20-22] These two inter-related and mutually complementing variables no doubt bridge the gap of other militating factors noted in the study, such as lack of information, distance to vaccination centres, poor access to media and lack of institutional deliveries. These two factors are also integrally associated with urban residence, which also favours greater uptake. More so, educated and wealthier women are more likely to have decision autonomy and appreciate the need for childhood vaccination.
Younger age group reducing the odds of vaccination of a child has been documented in another study in Nigeria.[23] This may be related to the experience of childcare and knowledge of the importance of vaccination that comes with increasing age.
Institutional delivery was associated with a higher rate of full immunisation uptake by children and has been shown to be highly correlated with access to maternal and child health services.[22] Access to media, as stated previously, usually is a reflection of maternal socioeconomic status and was also an important determinant in uptake. This has also been documented in other studies in Nigeria and other African countries.[24, 25] Finally, it was seen that the dropout rate for vaccines with a multiple dosing regimen increased with each successive dose. One could speculate that this could be related to the incidence of side-effects from previous doses and/or ignorance on the part of mothers who may believe that one dose of a particular vaccine type is enough.
Study limitations
Although the findings of this study are corroborated by those of other studies within and outside Nigeria, the results should be interpreted with caution in the light of the following limitations. Firstly, given the cross-sectional design of this study, some immunisation information obtained during data collection was by recall from the mothers, which is prone to recall bias. Secondly, several misclassifications may have occurred during categorisation, because mothers who skipped one vaccination, owing to medically permitted reasons, were considered under full vaccination uptake. Thirdly, paternal factors, community-level factors and other maternal factors that may have an influence on immunisation uptake were not considered in this study. Finally, the DHS usually does not collect data on variables such as full immunisation; these data were created by summing individual vaccine statuses. Maternal factors such as wealth index, religion and occupation were also computed from primary data given by the DHS. This recategorisation may have caused some misgrouping of individuals, causing potential errors in the analysis.
Conclusion
There is need for the Nigerian government and those in other developing countries, where vaccination rates are poor, to improve the socioeconomic status of its female citizens through better education and empowerment. Improved vaccination strategies are needed for the northern regions and rural communities of Nigeria. These strategies should involve and be acceptable to the communities in these locations. These measures, if effectively implemented, will possibly help improve coverage and vaccine uptake in Nigeria, and help to reduce deaths owing to vaccine-preventable disease.
Acknowledgements.We thank the officials of the Opinion Research Company (ORC) and the owners of the DHS for their kind assistance in permitting us to use the data used in this study. We also thank the Federal Ministry of Health and National Population Commission of Nigeria for their ethical clearance. The content of this study is the sole responsibility of the authors and is in no way representative of the official views of the ORC.
References
1. World Health Organization. Children: Reducing mortality. WHO. http://www.who.int/mediacentre/factsheets/fs178/en/ (accessed July 2012). [ Links ]
2. World Health Organization. Immunization surveillance, assessment and monitoring. http://www.who.int/immunization/monitoring_surveillance/en/ (accessed August 2012). [ Links ]
3. World Health Organization. Immunization coverage. http://www.who.int/mediacentre/factsheets/fs378/en (accessed July 2012). [ Links ]
4. World Health Organization. Immunization, surveillance, assessment and monitoring. Vaccine preventable disease. Available on www.who.int/immunization/monitoring/en (accessed May 2011). [ Links ]
5. United Nations International Children's Emergency Fund. Statistical and monitoring section, division of policy and practice 2011. Available at http://www.childinfo.org/files/32775_UNICEF.pdf (accessed July 2011). [ Links ]
6. World Health Organization. Immunization schedules in Nigeria, 2011. http://childsurvivalnetwork.info/resources/immunization+factsheet.pdf (accessed July 2011). [ Links ]
7. World Health Organization. Immunization schedule in Nigeria. In: Immunization Fact Sheet 2010. Geneva: World Health Organization, 2012. [ Links ]
8. Roberts KA, Dixon-Woods M, Fitzpatrick R, et al. Factors affecting uptake of childhood immunisation: A Bayesian synthesis of qualitative and quantitative evidence. Lancet 2002;360(9345):1596-1599. [http://dx.doi.org/10.1016/S0140-6736(02)11560-1] [ Links ]
9. Pruitt RH, Kline PM, Kovaz RB. Perceived barriers to childhood immunizations among rural populations. J Community Health Nurs 1995;12(2):65-72. [http://dx.doi.org/10.1207/s15327655jchn1202_1] [ Links ]
10. Schaffer SJ, Szilagyi PG. Immunization status and birth order. Arch Pediatr Adolesc Med 1995;149(7):792-797. [ Links ]
11. Odusanya OO, Ewan FA, Francois PM, Ahonkhai VI. Determinants of vaccination coverage in rural Nigeria. BMC Public Health 2008;8:381. [http://dx.doi.org/10.1186/1471-2458-8-381] [ Links ]
12. United Nations Population Division. World Population Prospects 2011 Revision. http://esa.un.org/wpp (accessed September 2012). [ Links ]
13. People and Ethnic Groups: CIA World fact book. http://www.cia.gov/library/publications/the-world-factbook/geos/ni.html (accessed July 2012) [ Links ]
14. Macro International. The DHS Program. Demographic and Health Surveys. Macro International. http://dhsprogram.com/ (accessed July 2011). [ Links ]
15. United Nations International Children's Emergency Fund. Immunization summary. A statistical referencing containing immunization data through 2011. http://www.childinfo.org/files/32775_UNICEF.pdf (accessed September 2011). [ Links ]
16. United Nations International Children's Emergency Fund. The Under-five Mortality Rate Fell by Almost Half Since 1990. http://data.unicef.org/child-mortality/under-five (accessed July 2011). [ Links ]
17. Jamison DT, Feachem RG, Makgoba MW, et al. Disease and mortality in subSaharan Africa. 2nd edition. Washington DC: World Bank, 2006:chapter 12. http://www.ncbi.nih.gov/books/NBK2284/. [ Links ]
18. Mancini L. Comparative trends in ethno-regional inequalities in Ghana and Nigeria: Evidence from Demographic and Health Survey. CRISE Working Paper No. 72 2009;7:10-11. [ Links ]
19. Oluwoye OR. Determinant of quality of rural life in Nigeria: The woman's view. Soc Indic Res 1990;22(3):227-286. [ Links ]
20. Antai D. Inequitable childhood immunization uptake in Nigeria: A multilevel analysis of individual and contextual determinants. BMC Infect Dis 2009;9:181. [http://dx.doi.org/10.1186/1471-2334-9-181] [ Links ]
21. Abdulraheem I, Onajole A, Jimoh A, Oladipo A. Reasons for incomplete vaccination and factors for missed opportunities among rural Nigerian children. Journal of Public Health and Epidemiology 2011;3(4):194-203. [ Links ]
22. Impicciatore P, Bosetti C, Schiavio S, Pandolfini C, Bonati M. Mothers as active partners in the prevention of childhood diseases: Maternal factors related to immunization status of preschool children in Italy. Prev Med 2000;31(1):49-55. [http://dx.doi.org/10.1006/pmed.2000.0677] [ Links ]
23. Antai D. Rural-urban inequities in childhood immunisation in Nigeria: The role of community contexts. Afr J Prm Health Care Fam Med 2011;3(1):238. [http://dx.doi.org/10.4102/phcfm.v3i1.238] [ Links ]
24. Doctor HV, Bairagi R, Findley SE, Helleringer S, Dahiru T. Northern Nigeria maternal, newborn and child health programme: Selected analysis from population based baseline survey. The Open Demography Journal 2011;4:11-21. [ Links ]
25. Owino B, John P. The Use of Maternal Health Care Services, Socio-economic and Demographic Factors: Nyanza, Kenya. University of Wisconsin, Centre for Demography and Ecology (CDE), 1998:108. [ Links ]
 Correspondence:
Correspondence:
O D I Chidiebere
chidi.osuorah@gmail.com













