Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671Print version ISSN 1994-3032
S. Afr. j. child health vol.14 n.2 Pretoria Jun. 2020
https://doi.org/10.7196/SAJCH.2020.v14i2.1670
RESEARCH
The effect of device position and use of transparent covers on the irradiance distribution of LED phototherapy devices
M T IsmailI; A R HornII
IMB ChB, FCPaed (SA); Department of Neonatal Medicine, School of Child and Adolescent Health, University of Cape Town, South Africa
IIMB ChB, DCH (SA), FCPaed (SA), Cert Neon (SA), PhD Department of Neonatal Medicine, School of Child and Adolescent Health, University of Cape Town, South Africa
ABSTRACT
BACKGROUND. Effective phototherapy reduces neonatal jaundice and its complications. Irradiance increases as the distance of the light source decreases from a single phototherapy light. There are limited studies of the effect of distance and positional changes on different light-emitting diode (LED) light designs on achieving effective phototherapy.
OBJECTIVES. To describe and compare the effect of distance, angle and plastic barriers on three different LED lights of different design.
METHODS. Comparisons were made using a Servolite, a General Electric (GE) Lullaby and a Ningbo David LED phototherapy light. Measurements were done according to methods described by the International Electrotechnical Commission (IEC). The effective irradiated area was measured on a grid measuring 60 x 30 cm subdivided into 5 x 5 cm squares. Measurements were done for the following scenarios: light placed at the manufacturer's recommended distance, 20 cm closer, 20 cm further, at an angle, through clear plastic and through scuffed Perspex.
RESULTS. When the lights were placed closer to the irradiated surface than the manufacturers' recommendations, the maximum irradiance increased, but the median irradiance and uniformity ratio decreased. When the lights were angled at 45°, the median irradiance was decreased. A decrease in the median irradiance was also seen when phototherapy lights passed through scuffed plastic and food-grade plastic.
CONCLUSION. Our study demonstrated that the placing of LED lights closer than the manufacturers' recommendations, the use of transparent barriers and the use of lights at an angle, compromised phototherapy irradiance and distribution. Only the GE light met IEC standards.
Neonatal jaundice (NNJ) occurs in the majority of healthy term and late-preterm newborns within the first week of life, owing to the accumulation of bilirubin in the blood.[1] Unconjugated bilirubin at high concentrations can cross the blood-brain barrier and cause bilirubin-induced neurological dysfunction (BIND), but effective phototherapy can prevent BIND.P1
Phototherapy using light wavelengths corresponding to the absorption spectrum of bilirubin in the blue-green spectrum peaking at 460±30 nm, reduces serum bilirubin.[3,4] Intensive phototherapy was defined by the American Academy of Pediatrics (AAP) in 2004 as irradiance in the 430 - 490 nm spectrum, of at least 30 μW/cm2/nm, 'measured at the infant's skin directly below the center of the phototherapy unit'l[5] The South African (SA) phototherapy guidelines recommend the use of intensive phototherapy when total serum bilirubin (TSB) exceeds time-dependent thresholds.[6] If bilirubin levels continue to rise despite phototherapy, the AAP guidelines suggest bringing phototherapy lights closer to the infant to increase irradiance.^ There are limited, device-specific studies showing a decrease in irradiance when a transparent barrier is placed between the neonate and the light source,[8-10] but neither the AAP nor the SA guidelines discuss the impact of transparent barriers. Despite the recommendations in the AAP guidelines, the manufacturers of light-emitting diode (LED) phototherapy devices in use at the authors' institution do not advocate using the device at a distance closer than the recommended distance; LED devices differ from older devices using fluorescent lights by having multiple small LED lights arranged with overlapping light cones. The device brochure for the General Electric (GE) Lullaby LED phototherapy light (GE Healthcare, Laurel, USA) states that the optical design ensures a uniform light distribution.[11] The focusing of the lights and strategic overlapping suggests that placement of LED devices closer to, or further away from, the infant will have a significant and probably negative effect on irradiance - different to the beneficial effect observed with fluorescent lights.
We hypothesised that placement of LED phototherapy devices closer than recommended by manufacturers will not achieve appropriate light intensity and distribution. We therefore aimed to compare the effect of phototherapy device position, distance and the presence of transparent barriers on the irradiance distribution maps of three devices frequently used in Cape Town, SA.
Objectives
1. To describe the irradiance distribution and the mean, maximum and minimum irradiance in the 420 - 480 nm spectrum in three LED phototherapy devices in the following situations:
• at the distance recommended by the manufacturer with the device horizontally aligned and at 20 cm higher and 20 cm lower
• at the distance recommended by the manufacturer with a mildy scuffed incubator Perspex hood between the device and the measuring radiometer
• at the distance recommended by the manufacturer with a single sheet of clear food-grade plastic bag between the device and the measuring radiometer
• at the distance recommended by the manufacturer with the device and aligned at an angle corresponding to the slope of an incubator.
2. To produce irradiance distribution maps for each of the devices and settings described above.
Methods
Study design and ethics approval
This was a bench-side observational study. The irradiance distributions of three phototherapy units were measured under different circumstances. The study was approved by the Paediatric Departmental Research Committee - approval from the Human Research Ethics Committee was not required because there were no human or animal participants.
The devices (the study sample)
Three new LED phototherapy devices were supplied by the distributors for comparison:
1. a Servolite (SL) LED phototherapy light (Servocare Medical Industries, South Africa (SA)), with five focused high-power blue LED lights producing overlapping light cones
2. a General Electric (GE) Lullaby LED phototherapy light (GE Healthcare, USA) with two separate clusters of high-power blue LED lights that produce two beams which overlap in the middle of the irradiated area
3. a Ningbo David (ND) XHZ-90L LED light (Ningbo David Medical Device Company, China) with multiple blue LEDs spaced to create a broad beam of light.
These devices were chosen as they were in the most frequent use in the authors' neonatal services. They also represent different styles of LED orientation. The irradiance of the devices was measured in several different scenarios that are frequently encountered in clinical practice. The distances recommended by the manufacturers for each device listed above are: 50 cm, 35 cm and 50 cm, respectively.
Data collection (irradiance measurement)
We used the standardised method of measuring irradiance distribution described by the International Electrotechnical Commission (IEC).[12] The IEC defines the effective irradiated area (EIA) as the 'intended treatment surface which is illuminated by phototherapy'. Previously, the EIA was referred to as the effective surface area (ESA). The IEC recommends an EIA of 60 cm x 30 cm with irradiance measurements on a grid with 10 cm or less separating each measurement. The EIA is further defined by the IEC as the area whereby the ratio of minimum irradiance to maximum irradiance, the uniformity ratio (UR), is >40%. Irradiance should be measured with the phototherapy device at the height and position recommended by the manufacturer. Hence, the IEC recommends a desired value for minimum irradiance of 0.4 x maximum irradiance to ensure uniformity of irradiance.
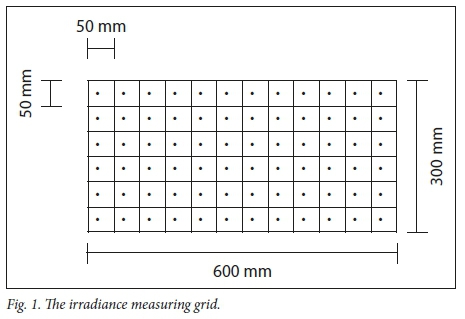
We placed a 60 x 30 cm template, with a grid of 5 cm squares (Fig. 1) on the surface where irradiance was measured. Irradiance was measured using the Ohmeda Medical BiliBlanket Meter II (GE Healthcare, USA). This radiometer measures a spectral range of 400 - 520 nm with a centre wavelength of 450 nm and a bandwidth of 60 nm. The measuring range of its spectral irradiance is 0.1 - 2 99.9 μW/cm2/nm. The manufacturer states that the device can be used to measure irradiance from LED, fluorescent, halogen and fibre-optic phototherapy devices. The Ohmeda radiometer was the preferred device for irradiance assessment by GE Healthcare - the manufacturers of the other two devices did not specify a preference in their brochures. Irradiance was measured by placing the radiometer in the centre of each square on the grid with the phototherapy device directed on it in different situations, as described below. The values obtained were recorded on a hard-copy grid and then entered into an Excel (Microsoft Corp., USA) spreadsheet with columns and rows labelled according to their position on the measuring grid.Vreman et al.[13] recommend measuring and plotting irradiance over a rectangular grid of 50 x 30 cm. They also recommend assessing irradiance over a silhouette of a term infant placed in the centre of the bed, with approximate length of 40 cm and approximate greatest width of 20 cm, to determine the percent treatable body surface area (BSA).[14]
Irradiance was measured for each device in the following scenarios:
1. The device was positioned above the middle ofthe grid, in the same position that it would be if the grid was enclosed in an incubator, horizontally orientated, using a spirit level, with no obstructions. Irradiance was measured at the height recommended by the manufacturer, at 20 cm higher (far position) and 20 cm lower (close position), measured with measuring tape and a plumb line from the centre of the device to the centre of the grid.
2. The device was positioned as above at the height recommended by the manufacturer with a single layer of food-grade clear plastic covering the light meter (but not touching it).
3. The device was positioned over a mildly scuffed incubator, the grid was placed on the mattress of the incubator, the light centred over the middle of the grid, horizontally orientated, at the height recommended by the manufacturer.
4. The device was positioned centrally but slightly to one side as it would be on the side of a closed incubator, orientated at an angle of 45 degrees, with no obstructions, at the height recommended by the manufacturer. The position as it would be with a closed incubator is shown in Fig. 2.
Data analysis
Stata Version 12 (StataCorp., USA) was used for statistical analysis. The mean, median, maximum and minimum irradiances and the UR were calculated for each scenario over the 60 x 30 cm grid and also when the EIA was decreased to 50 x 30 cm and 40 x 20 cm. Irradiance was represented graphically as a map or 'footprint' for each scenario. Since several data distributions within the light footprints were not symmetrical, median irradiance was compared using the Wilcoxon signed-rank test for matched samples.
Results
Measurements over an EIA defined by a 60 x 30 cm grid (1 800 cm2)
The irradiance measurements over the entire 60 x 30 cm grid for each device and setting are shown in Table 1 and Figs 3 - 5.
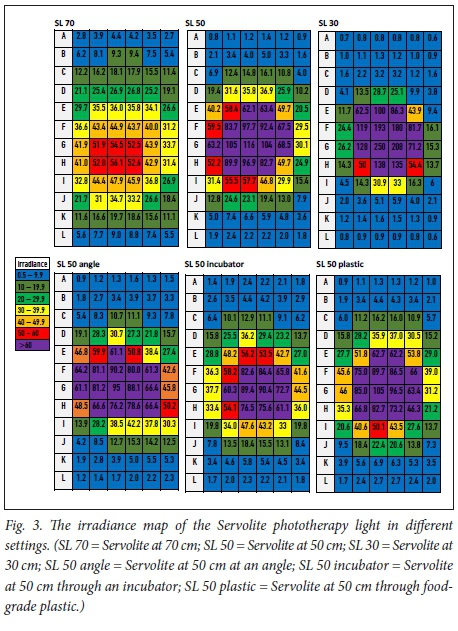
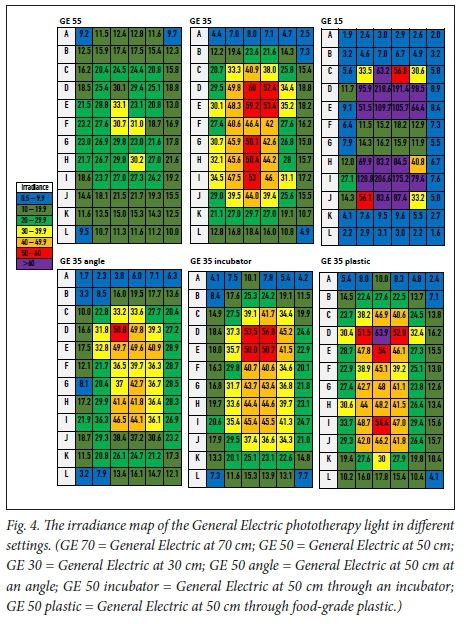
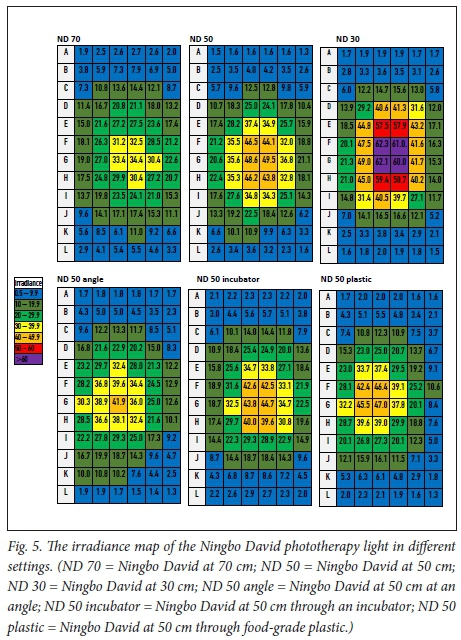
The frequent differences between mean and median irradiances demonstrate the non-normal distribution of the data. Minimum irradiance was below 2 μW/cm2/nm for all devices when positioned at the recommended distance. The UR was substantially less than 0.4 in all cases and it decreased further as lights were brought closer. When the devices were placed 20 cm closer than manufacturers' recommended distances (close position), the maximum and mean irradiance increased, and the median irradiance decreased compared with the mean irradiance, but the minimum irradiance decreased in all cases except the ND. The maximum irradiances at the close position were very high and ranged from 60 - 249.8 μW/cm2/nm. All devices showed a very rapid fall-off in irradiance around the edges of a small high-intensity area when placed at the close position. When the GE was placed at the close position, this resulted in two separate small high-intensity patches of irradiance separated by very low irradiance between (Fig. 4).
When the lights were angled at 45°, the maximum irradiance decreased with the SL and GE, but increased with the ND. In this position, the median irradiance decreased by 27.8%, 7.6% and 13.9% in the SL, GE and ND, respectively. There was a marginal decrease in median irradiance when phototherapy light passed through mildy scuffed incubator plastic of 3.7%, 3.1% and 0.7% in the SL, GE and ND respectively - and maximum irradiance decreased in all devices. A single layer of food-grade plastic decreased the irradiances by 10.8%, 0.4% and 27.8% in the SL, GE and ND respectively - maximum irradiance decreased with the SL and ND but was marginally increased with the GE
Measurements over an EIA of 50 x 30 cm (1 500 cm2)
The irradiance measurements when EIA is defined as 50 x 30 cm are shown in Table 2. The irradiance map for this area can be appreciated in Figs 3 - 5 by ignoring the first and the last rows. The maximum irradiance was the same as for the 60 x 30 cm grid, but minimum irradiance and UR only increased marginally. The only device with UR >0.4 was the GE - at the far position. The UR for both the SC and the ND were highest at the far distance - and the minimum irradiance was highest at the far distance for these devices. The median irradiance was unchanged or decreased when transparent barriers were in place; the decrease ranged from 0 - 21%.
Measurements over an EIA of 40 x 20 cm (800 cm2)
The irradiance measurements when EIA is defined as 40 x 20 cm are shown in Table 3. The pattern of variation in irradiance for these areas can be seen in Figs 3-5; the 40 x 20 cm area is obtained by ignoring the first two rows, the last two rows and the first and the last columns. The maximum irradiance was the same as for the 60 x 30 cm grid. The minimum irradiance and URs increased further compared with the 50 x 30 cm grid, but the GE was still the only device with UR >0.4 - at all positions except the close position and when plastic covered the radiometer. The UR and the minimum irradiances for both the SC and the ND were again highest at the far distance. The changes in irradiance with devices angled at 45 degrees were similar to those observed over the larger grids, but larger changes in irradiance were observed with transparent barriers in place. Decrease in irradiances through incubator plastic were: 18.2%, 7.2% and 7% for the SL, GE and ND, respectively. Decreases in irradiance through food-grade plastic were: 8.3%, 2.1% and 20.2% for the SL, GE and ND, respectively.
Discussion
Three different LED phototherapy lights were chosen for the study based on their frequency of use and their design. The designs included overlapping beams from clustered LEDs, focused beams from overlapping light cones, and multiple LEDs spaced out to create a broad beam of light.
The present study demonstrates that the distribution of irradiance intensity changes substantially when placing these LED phototherapy devices 20 cm closer or further away from the target treatment surface. Placing the devices 20 cm closer than recommended by the manufacturers resulted in a large increase in maximum irradiance, but minimum irradiance was decreased to levels well below 8-10 μ\ν/«η2/ηπι in peripheral areas and, in the case of the GE device, also in the central area of the light footprint - these decreases resulted in a substantial reduction of the effective irradiated area. Irradiance intensity changed by over 100 μ\ν/«η2/ηπι within as little as 5 cm in several cases but there was wide variation between the devices. The placement of incubator or food-grade plastic between the device and the therapeutic target had marginal effect on maximum irradiance but decreased median irradiance in all devices over 40 x 20 cm grid by up to 20%. There were similar changes when using the device at an angle, but the maximum irradiance increased by over 80% with the ND.
The IEC do not stipulate a minimum or maximum irradiance, since the optimal irradiance of phototherapy has not yet been established.[12] An irradiance of 8 - 10 μW/cm2/nm was defined by the AAP in 1994 as 'standard phototherapy' - this was based on the irradiance of 'conventional' or 'standard daylight units' at a distance of 20 cm.[15] The AAP recommend standard phototherapy when bilirubin levels are 34 - 51 μmol/L below the threshold for intensive phototherapy.[1,15] The AAP 2004 guidelines suggest that optimal irradiance is 30 μW/cm2/nm, also referred to as 'intensive phototherapy' - based on data at the time suggesting that higher intensities would not be effective at lowering bilirubin levels.[5] However, previous and more recent studies using LED phototherapy lights have shown a linear correlation between light irradiance at 5 - 55 μW/cm2/nm and percentage change in serum bilirubin - the linear relationship suggests that saturation will not occur at higher doses.[3,4] Hence, doses of 30 - 55 μW/cm2/nm may be considered optimal, spread evenly over the surface of the neonate with UR >0.4.
The practice of bringing phototherapy lights closer was recommended at the time when special blue fluorescent bulbs were commonly in use.[5] Light intensity with these lights is inversely related to distance from the source and, when these lights are moved closer to infants, serum bilirubin falls more rapidly.[16] The National Institute for Health Care and Excellence (NICE) guidelines, developed in the United Kingdom and updated in 2016, do not refer to 'optimal' or 'intensive' phototherapy - they refer only to 'phototherapy' and 'intensified phototherapy' without defining these terms with irradiance measures.[17] They suggest 'increasing the irradiance of the original light source' or adding more lights, and they state that phototherapy devices should be used according to manufacturers' instructions.
Although a randomised trial of aggressive v. conservative phototherapy in preterm infants showed improved neurodevelopmental outcomes with aggressive phototherapy and no significant effect on death,[18] there are concerns that prolonged phototherapy may be associated with DNA damage; the occurrence of very high irradiances focused on small areas when placing the devices close may not be safei[9] A preferable approach may be to select a higher-intensity setting (if the device offers it). Alternatively, additional lights could be added so that the lights remain focused in the optimal position, increased surface area of skin is exposed, and there is a more uniform increase in irradiance. This is a topic for further study.
The large variation in irradiance intensities when phototherapy devices are moved very close to the therapeutic target is further demonstrated by very low UR. The UR >0.4 required by the IEC precludes the use of any devices we studied in the close position.[12] When used at recommended distances, only the GE device achieved this ratio in our study, and only over an EIA of 40 x 20 cm.
UR decreases with decreasing size of the EIA. Treatment of babies smaller than this size is expected to be associated with improved UR and higher minimum irradiance. The ND and SL (at 50 and 70 cm, respectively) may provide irradiance at levels in line with IEC recommendations when applied to the smaller area of a preterm baby - this concept should be explored in further research.
Several methods of assessing irradiance, other than those ofthe IEC and Vreman, have been recommended.[20-22] Dicken et al.[20] measured irradiance levels over a rectangular area, based on the assumption that one-third of skin surface area is available for treatment - irradiance was measured over 20 cm x 35 cm for term neonates. Subramanian et al.[21] recommended measuring irradiance at 5 cm intervals over a rectangular grid of 60 cm x 30 cm and then tracing onto the grid an outline of a term baby with a two-dimensional surface area of 780 cm2 to determine the BSA. Irradiance was measured at the centre and at four peripheral points and maximum, minimum and mean irradiance were measured within the outline of the neonate. Reda et al.[22] recommended measuring and plotting irradiance at 7.5 cm intervals over a rectangular grid of 60 cm x 30 cm. We did not use an infant silhouette and we did not calculate treatable BSA, because the measurement of treatable BSA assumes that the infant lies still throughout treatment and that light approaches in a single plane, which is not the case. This method is also complex and the actual size of the silhouette and minimum irradiance to define 'treatment' have not been clearly defined, making it a difficult method to reproduce. Instead, we measured irradiance parameters over a 40 x 20 cm area, which is similar to the rectangular space occupied by a baby, is the area that lights are focused around in practice, and is also similar to the area described by Dicken et al.[20]
In addition to irradiance variation with height, the presence of physical barriers to light around neonates can also have an effect. Phototherapy irradiance provided with fluorescent bulbs decreases with the use of plastic blankets and heat shields.[8-9] A decrease in irradiance has also been described when phototherapy is applied through a scratched incubator surface.[10] Our data with LED lights are similar.
The present study has several limitations. Each irradiance measurement was only taken once. However, 72 measurements were taken on each grid and the consistency of measurement can be appreciated from the irradiance maps (Figs 3 - 5). The operation and maintenance manual states that the Ohmeda Medical BiliBlanket Meter II measures irradiance continually with an accuracy of ~3%. We performed a post hoc evaluation of accuracy by taking 72 measurements (the number of measurements in each grid) in the same position. The mean (standard deviation) of 72 measurements taken at 35 cm below the centre of the Lullaby device was 39.6 (0.1) μW/cm2/nm. Further limitations are: only one device of each type was evaluated; and the distance between the plastic cover and the light source may have had a more profound effect than we observed without the cover. The positions used were based on what is done in clinical practice.
Conclusion
We have demonstrated that the most appropriate distance to place LED phototherapy lights depends on the design of the lights. Placing lights closer than recommended significantly compromises the light distribution and irradiance. The use of transparent barriers decreases irradiance further. All three lights had maximum irradiance of at least 30 uW/cm2/nm (sufficient for intensive phototherapy) at all the distances, but minimum irradiance was only >8 uW/cm2/nm (sufficient for standard phototherapy) for most devices over the small grid of 40 x 20 cm. The UR only met IEC-recommended standards with the GE light. The SL device had improved uniformity with acceptable irradiance when used at 70 cm rather than the recommended 50 cm.
Although the GE device is the only device that meets both IEC and AAP recommendations for standard and intensive phototherapy, it only does so over a 40 x 20 cm grid. There is no evidence to show that the use of device with uniformity ratios <0.4, very high maximum irradiance and low minimum irradiances below 8 uW/cm2/nm is associated with unacceptable performance.
Clinicians should be aware of the recommended distance and the shortcomings of phototherapy devices. Further research is needed to (i) evaluate consistency of performance between devices from the same manufacturer; (ii) determine the effect that distance and angle have on irradiance when barriers are used; (iii) determine the effect on irradiance of using more than one light; and (iv) determine simple rapid bedside irradiance assessment methods. The terms 'intensive' and 'standard' are misleading and poorly defined - there is a need to establish more appropriate terms that adequately describe the dose of phototherapy being given.
Declaration. This manuscript is the work of both authors without input from any other parties. It has not been published anywhere else in any other format, but it will form part of a Master of Medicine (Paed) degree.
Acknowledgements. Thanks to Medhold Medical for the loan of the radiometer and the donation of a GE Lullaby LED phototherapy light for continued use after the study.
Author contributions. MTI wrote the protocol, collected the data, participated in data analysis and result interpretation and wrote the manuscript. ARH conceptualised the study, supervised all aspects of the study, assisted with data analysis and interpretation, and critically reviewed the manuscript.
Funding. Supported in part by a research grant from the Health Sciences Faculty, University of Cape Town.
Conflicts of interest. The radiometer used to measure irradiance was supplied by Medhold Medical (Pty) Ltd - a distributor of the GE Lullaby LED phototherapy light.
References
1. Maisels MJ, McDonagh AF. Phototherapy for neonatal jaundice. N Engl J Med 2008;358(9):920-928. [ Links ]
2. Watchko JF, Tiribelli C. Bilirubin-induced neurologic damage - mechanisms and management approaches. N Engl J Med 2013;369(21):2021-2030. https://doi.org/10.1056/nejmra1308124 [ Links ]
3. Tan KL. The pattern of bilirubin response to phototherapy for neonatal hyperbilirubinaemia. Pediatric Research 1982;16(8):670-674 [ Links ]
4. Vandborg PK, Hansen BM, Greisen G, Ebbesen F. Dose-response relationship of phototherapy for hyperbilirubinemia. Pediatrics 2012;130(2):e352-357. https://doi.org/10.1542/peds.2011-3235 [ Links ]
5. Subcommittee on hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 2004;114(1):297-316. https://doi.org/10.1542/peds.114.L297 [ Links ]
6. Horn AR, Kirsten GF, Kroon SM, et al. Phototherapy and exchange transfusion for neonatal hyperbilirubinaemia: Neonatal academic hospitals' consensus guidelines for South African hospitals and primary care facilities. S Afr Med J 2006;96(9):819-824. [ Links ]
7. Maisels MJ. Why use homeopathic doses of phototherapy? Pediatrics 1996;98(2 Pt 1):283-287. [ Links ]
8. Stutchfield PR, Modi N, Weindling AM. Phototherapy and the use of heat shields in very low birthweight infants. Arch Dis Childhood 1988;63(5):552-554. [ Links ]
9. Bayliss SC, Moseley MJ, Hobbs B, Curnock DA. Phototherapy and the use of heat shields. Arch Dis Childhood 1988;63(10):1295-1296. [ Links ]
10. Chien CH, Tsou Yau KI. The influence of incubator wall on the irradiation intensity of phototherapy. Zhonghua Minguo xiao er ke yi xue hui za zhi [journal] 1996;37(2):92-95. [ Links ]
11. Lullaby LED Phototherapy System. Product brochure. http://www3.gehealthcare.com.au/~/medi a/do wnloads/anz/pro duct s/maternal-infantcare/phototherapy/lullaby-led-pt-brochure-anz-doc0995660.pdf?Parent-%7BA2EAE056-7761-4244-A36C-92E3D711BF25%7D (accessed 10 July 2019). [ Links ]
12. I E Comission. Medical Electrical Equipment - Part 2-50: Particular Requirements for the Safety of Infant Phototherapy Equipment. IEC 60601- 2-50: 2009+AMD 1:2016 CSV 2016; Edition 2.1 (2016-04):1-126. Geneva: IEC, April 2016. [ Links ]
13. Vreman HJ, Wong RJ, Murdock JR, Stevenson DK. Standardised bench method for evaluating the efficacy of phototherapy devices. Act Paediatr 2008;97(3):308-316. https://doi.org/10.1111/j.1651-2227.2007.00631.x [ Links ]
14. Cline bK, Vreman HJ, Lou HH, Donaldson KM, Bhutani VK. Evaluation of an affordable LED phototherapy device for resource-limited settings. Pediatric Academic Societies Conference, Denver, Colorado, 30 April - 3 May 2011. [ Links ]
15. Subcommittee on hyperbilirubinemia. Practice parameter: Management of hyperbilirubinemia in the healthy term newborn. Provisional Committee for Quality Improvement and Subcommittee on Hyperbilirubinemia. American Academy of Pediatrics 1994:558-565. [ Links ]
16. Modi N, Keay AJ. Phototherapy for neonatal hyperbilirubinaemia: The importance of dose. Arch Dis Childhood 1983;58(6):406-409. [ Links ]
17. Amos RC, Jacob H, Leith W. Jaundice in newborn babies under 28 days: NICE guideline 2016 (CG98). Arch Dis Child Educ Pract 2017;102(4):207-209. https://doi.org/10.1136/archdischild-2016-311556 [ Links ]
18. Morris BH, Tyson JE, Stevenson DK, et al. Efficacy of phototherapy devices and outcomes among extremely low birth weight infants: Multi-center observational study. J Perinatol 2012;33(2):126-133. https://doi.org/10.1038/jp.2012.39 [ Links ]
19. Ramy N, Ghany EA, Alsharany W, et al. Jaundice, phototherapy and DNA damage in full-term neonates. J Perinatol 2016;36(2):132-136. [ Links ]
20. Dicken P, Grant LJ, Jones S. An evaluation of the characteristics and performance of neonatal phototherapy equipment. Physiological Measurement 2000;21(4):493-503. [ Links ]
21. Subramanian S, Sankar MJ, Deorari AK, et al. Evaluation of phototherapy devices used for neonatal hyperbilirubinemia. Indian Pediatr 2011;48(9):689-696. https://doi.org/10.1007/s13312-011-0116-8 [ Links ]
22. Reda SM, Yasmen AEB. Performance evaluation for hyperbilirubinemia phototherapy equipment. Aust J Basic Appl Sci 2013;7(9):364-366. [ Links ]
 Correspondence:
Correspondence:
A R Horn
alan.horn@uct.ac.za
Accepted 15 August 2019.