Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Journal of Radiology
On-line version ISSN 2078-6778Print version ISSN 1027-202X
S. Afr. J. radiol. (Online) vol.21 n.1 Johannesburg 2017
https://doi.org/10.4102/sajr.v21i1.1191
ORIGINAL RESEARCH
Dynamic ultrasound evaluation of the syndesmosis ligamentous complex and clear space in acute ankle injury, compared to magnetic resonance imaging and surgical findings
Chantelle van Niekerk; Barbara van Dyk
Department of Medical Imaging and Radiation Sciences, University of Johannesburg, South Africa
ABSTRACT
BACKGROUND: Syndesmosis injuries are often more serious than an injury to the lateral ligament complex of the ankle, with double the recovery time, chronic discomfort and joint instability. Although magnetic resonance imaging (MRI) is considered as the best imaging modality to assess the integrity of the syndesmotic ligamentous complex and clear space, a dynamic ultrasound evaluation may provide an alternative imaging option worthy of exploring
AIM: The aim of this article is to compare the sensitivity and specificity of musculoskeletal ultrasound and MRI, in the diagnosis of syndesmosis pathology, with surgical findings as the reference point
METHOD: MRI was performed on 114 participants presenting with pain over the lateral aspect of the ankle after injury. This was followed by a dynamic ultrasound examination during which the anterior tibiofibular ligament (ATiFL) was assessed for continuity, contour and haematoma. The tibiofibular clear space was measured with the ankle in a neutral position, followed by internal and external rotation
RESULTS: The Fisher's exact test was used to determine non-random associations between variables and compute statistical significance (p < 0.05). Ultrasound achieved a sensitivity of 86.3%, specificity of 97% with a false-positive rate of 3%. The sensitivity of MRI is similar to that of ultrasound (86%) with a specificity of 100%
CONCLUSION: Although both imaging tests performed very well, MRI was slightly better at excluding pathology while both tests performed equally in demonstrating pathology. As a simple, inexpensive and reproducible test, dynamic ultrasound can thus be considered as an alternative to MRI in acute ankle pathology
Background
Magnetic resonance imaging (MRI) is currently considered to be the best imaging modality for the diagnosis of acute soft tissue and intra-articular ankle pathology. In contrast, musculoskeletal (MSK) ultrasound is a rapidly evolving speciality which is playing a major role in the diagnosis and management of soft tissue injuries, especially in sports medicine.1 Continuous technological advances in ultrasound imaging have enabled the detection of previously imperceptible soft tissue pathology and ligamentous structures with great clarity.1 Most importantly, ultrasound facilitates dynamic real-time imaging of MSK structures, during which the patient is able to guide the sonographer to the point of maximum tenderness, allowing for a thorough examination of the area of concern.2
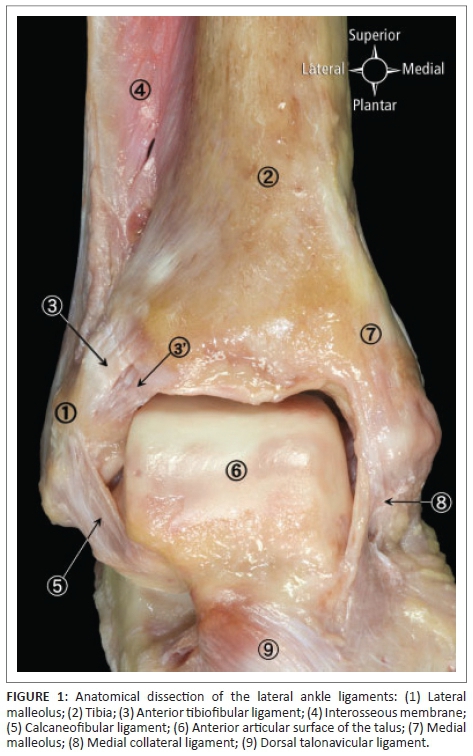
Once ligaments have been seriously or permanently damaged, they are unable to stabilise the joint and protect it from excessive motion. The syndesmotic ligamentous complex plays a significant role in the stabilisation of the ankle joint (Figure 1)3. The function of these ligaments is to secure the tibia and fibula close together in order to prevent abnormal widening of the ankle mortise. Although the anterior tibiofibular ligament (ATiFL) is the main structure in preventing excessive movement of the fibula and external rotation of the talus, it is also the most vulnerable to syndesmotic ankle sprains.4,5,6 Syndesmotic injuries involve disruption of the ligamentous structures between the distal fibula and tibia. Rupture of the ATiFL will, thus, result in instability of the ankle mortise, demonstrated as widening of the tibiofibular clear space (Figures 2 and 3)8,11 which predisposes to chronic dysfunction.4,7

The tibiofibular clear space represents the distance between the lateral border of the posterior tibial prominence and the medial border of the distal fibula. Likewise, the tibiofibular overlap indicates the maximum distance between the antero-lateral border of the distal tibial prominence and the medial border of the distal fibula. When measured 1 cm above the tibial plafond, the normal tibiofibular clear space should be < 6 mm while the normal tibiofibular overlap is > 1 mm for the mortise view (Figures 2 and 3).8,9,10
Table 1 summarises the radiographic criteria for the diagnosis of a syndesmosis injury.11
The severity of syndesmosis injuries ranges from simple isolated sprains to more complex ligamentous injuries with associated fractures.6 An injury to the syndesmosis is, therefore, usually more serious than an injury to the lateral ligament complex of the ankle with double the recovery time. Syndesmotic injuries are also more prone to chronic discomfort and instability; as such injuries result in diastasis and abnormal joint motion.12 It is, however, difficult to recognise syndesmotic injuries in the absence of a fracture or diastasis and, hence, high ankle sprains can easily go undiagnosed. Despite controversy regarding the appropriate treatment of syndesmotic injuries, options should be considered with caution as treatment will determine the functional outcome of the patient.13
A simple, fast, yet reliable diagnostic imaging test is, therefore, desirable to assess the integrity of the distal tibiofibular syndesmosis. Although superficial soft tissue structures can now be imaged with great clarity, ultrasound is still only occasionally regarded as the imaging modality of choice because of referring specialists' personal preferences and non-availability of qualified sonographers with expertise in MSK ultrasound.14 Until recently, there was paucity in the literature regarding the ability of high-frequency ultrasound to determine acute syndesmosis pathology accurately.1,15 The evolution of MSK ultrasound, therefore, sparked the evaluation of MSK ultrasound's diagnostic ability to accurately determine syndesmosis injury when compared with MRI and surgical findings. Consequently, the aim of this article is to compare the sensitivity and specificity of MSK ultrasound and MRI to demonstrate acute pathology of the syndesmotic ligamentous complex, with surgical findings as the reference point, and correlate our findings with recent literature.
Methods
MRI examinations were performed using a 3-Tesla magnet (Intera, Phillips Medical Systems) with a 20 cm wrap around ankle and/or foot coil. The injured foot was placed in a fixed neutral position and steadied with Velcro straps. T1- and T2-weighted images were obtained in the axial, coronal and sagittal planes. A field of view of 10 cm was used with a slice thickness of 4 mm on the axial image plane and 3 mm for the sagittal and coronal planes. A bandwidth of 20 kHz, and 224 × 224 matrix were used for all sequences. The MRI sequences were as follows: sagittal, T1-weighted, spin-echo [500 ms - 600 ms repetition time (TR), 12 ms - 17 ms echo time (TE)], proton density (2000 ms TR/15 ms TE) and fat-suppressed T2-weighted, fast spin-echo (3000 ms - 4000 ms TR/60 ms TE). The total acquisition time was approximately 20 min - 30 min. However, if sub-optimal images were obtained with the standard protocol, an additional sequence was performed to ensure optimal visualisation of the ATiFL in its entire length. For this sequence, the ankle was positioned at 45° inversion. MR images were reported with the aid of a standardised template allowing comment on the ATiFL and syndesmosis.
The ultrasound examination was performed at no additional cost to the patient. Both ankles were examined for comparative purposes, using a Toshiba Aplio 500 ultrasound unit boasting a high resolution, multi-frequency (7 MHz - 15 MHz) linear transducer. Ultrasound examinations were, likewise, performed according to a set protocol allowing optimal visualisation of anatomical structures.16 The patient was seated on the examination table with the knee in 90º flexion and the plantar aspect of the foot in full contact with the table (Figure 4).
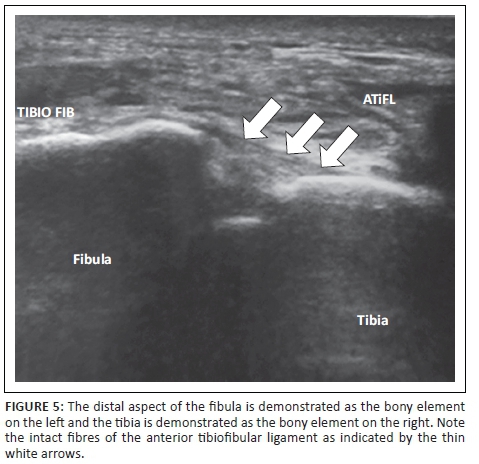
The transducer was placed transversely over the lateral aspect of the foot approximately 1 cm proximal to the ankle joint where the ligament is the thickest, while the posterior aspect of the transducer was placed just distal to the lateral malleolus. The squeeze test was performed during real-time imaging by pressing the tibia and fibula towards each other at the level of the mid-calf. With a syndesmosis injury, this manoeuvre elicits pain distally at the level of the distal tibiofibular syndesmosis.17 In order to evaluate the ATiFL for continuity, contour and haematoma formation, the anterior aspect of the transducer was rotated cranially and obliquely until the distal fibula and ATiFL were visible (Figure 5).
Images of the anatomical landmarks of the syndesmosis were obtained with the foot in neutral position (Figure 4) as well as in internal rotation. The cine loop facility enabled scroll back of the last frames to identify the image which demonstrated the maximum clear space distance. The tibiofibular clear space was measured at the deep border of the ligament, from the distal aspect of the fibula to the bony surface of the tibia, over the antero-lateral aspect of the ankle (Figure 6).

Subsequently, the patient was requested to press the heel towards the bed and to dorsiflex the foot as much as possible in order to best stabilise the ankle. Thereafter, the patient was asked to place the foot in maximum external rotation with the knees close together, while maintaining 90° knee flexion (Figure 7).
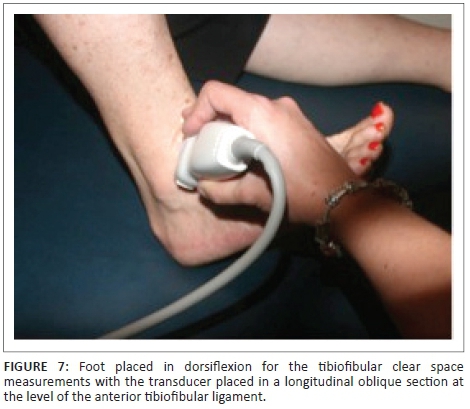
Additional force was then applied to further externally rotate the foot, thus achieving forced eversion. The clear space measurement was repeated with the foot in dorsiflexion and forced external rotation (Figures 8 and 9).12

Statistical analysis
Data analysis was conducted using SPSS version 22 software. Descriptive statistics employed frequency tables to describe the sample while cross tabulations were employed to present inferential statistics and effect sizes. The Fisher's exact test was used to determine non-random associations between two categorical variables and analyse statistical significance in a small sample size (p < 0.05), while the Phi test was used as a post-test to determine the effect size with a value between 0 and 1. The Kappa's measure of agreement calculated the interrater reliability between the different variables, and sensitivity and specificity were subsequently determined and displayed as a ROC curve.
Results
Biographical characteristics of the sample are summarised in Tables 2 and 3.
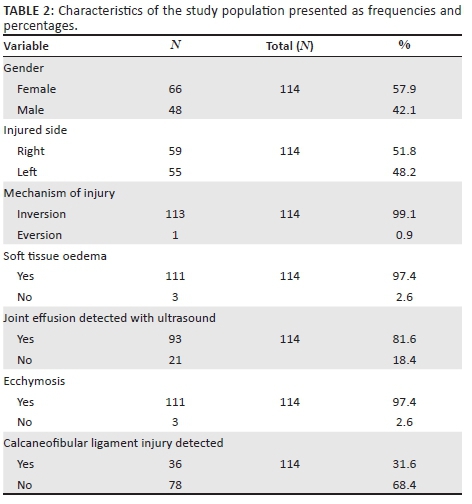
From a total of 114 participants, 58% were female and 42% were male, while 52% presented with a right ankle injury. The age of the participants varied from 11 to 69 years with a mean of 33.8 years. The mechanism of injury was eversion for a single (1%) participant. Ecchymosis and subcutaneous soft tissue oedema was noted in 97% of the cases while ultrasound revealed a joint effusion in the anterior joint space in 82% of the cases. Avulsion fractures were incidentally detected in 12 (11%) participants and injury to the calcaneofibular ligament (CFL) was noted in 32% of the participants.
Table 4 demonstrates the sonographic evaluation of the tibiofibular clear space with the foot placed in different positions.
The mean clear space measurement in injured ankles (5.7 mm) increased in external rotation (ER) with a mean of 1 mm when stress was applied. In contrast, the mean clear space measurement in non-injured ankles was 5.3 mm, with a mean increase of 0.6 mm with stress.
In Table 5, a comparison is made between MSK ultrasound, MRI and surgical findings.
Table 5 demonstrates that MRI classified 70 syndesmoses as normal and 44 as abnormal while surgery confirmed that 63 patients had a normal syndesmosis with 51 being injured. MRI, therefore, missed seven syndesmosis injuries. With p = <0.00 (Fisher's Exact) and a Kappa value of 0.874, there is a statistically significant difference with a large association between MRI and surgical findings, with the null hypothesis being rejected.
Ultrasound classified 68 participants as normal and 46 as abnormal. Ultrasound, therefore, missed five syndesmosis injuries and classified two normal syndesmoses as pathological. With p < 0.00, a Phi value of 0.842 and a Kappa measure of agreement of 0.839, a statistically significant result was obtained with a large association.
A good diagnostic test demonstrates small false-positive and false-negative rates across a range of cut off values. It is ideal when the ROC curve displays a rapid climb towards the upper left hand corner of the graph. The ROC curve in Figure 10 illustrates the sensitivity and specificity of MSK ultrasound and MRI findings when compared with surgical results. Although both tests rendered good results, the false-positive rate for ultrasound is minimally (3%) higher than that obtained from MRI while the false-negative rate for both tests was 13.7%.

Ethical considerations
A quota non-probability sampling method was employed in this comparative descriptive study by recruiting participants from a population of patients with acute ankle injuries. This rigorous form of sampling ensured representativeness of the population by inviting all injured patients who presented with pain over the lateral aspect of the ankle, and had been referred for an MRI, to participate in the study. Participation was voluntary and after an explanation of the study purpose, all participants provided written consent. Approval for the study was obtained from the Higher Degrees and Research Ethics Committees of the Faculty of Health Sciences, University of Johannesburg (HDC47-01-2012) and the Ethics Committee of the hospital group where the study was conducted (UNIV-2013-0001).
Discussion
The purpose of this study was to confirm the ability of MSK ultrasound to accurately diagnose acute injury to the ankle syndesmosis when compared with MRI and ultimately surgical results. MRI is currently regarded as the imaging modality of choice because of the comprehensive evaluation of intra-articular structures, bony and osteochondral lesions, ligament and tendon pathology and synovitis. Furthermore, it facilitates grading of a ligamentous injury according to severity.1 Surgical findings are, however, considered as the diagnostic gold standard, given the direct visualisation of the anatomical structures.1
When ultrasound and MRI findings were compared, a dissimilarity was found in 12 participants. The divergence was cleared through comparison with the surgical findings, with MRI achieving a marginally better score than ultrasound in the identification of true negative findings. A negligible difference of 3% was recorded between the sensitivity and specificity values of MRI and ultrasound, respectively, with MRI being better at excluding pathology and ultrasound being equal to MRI at demonstrating pathology.
In this study, the mean normal tibiofibular clear space measured N = 5.3 mm, IR = 5.2, ER = 5.9 while a mean of 5.7 mm was recorded in injured ankles. This is significantly larger than the mean measurements recorded for normal ankles in an Israeli population (N = 3.7 mm, IR = 3.6 mm and ER = 4.0 mm)17 in spite of their study sample being comparable to ours in age. The authors concluded that a measurement of 5.06 mm obtained in a neutral position would represent two standard deviations above the mean, suggestive of an abnormal finding. This implies that the normal values for the Israeli population cannot be generalised to a South African population.
Dynamic ultrasound evaluation of the syndesmosis resulted in a mean clear space widening of up to 1.0 mm with external rotation (mean 0.6 mm) with no correlation between gender, age, activity or height. The mean increase in anterior clear space with stress application (ER-N) was found to be 0.3 mm in the Israeli study, with a significantly wider clear space opening in forced external rotation in females. This agrees with the literature as female subjects tend to be more flexible than males.18
Our study further demonstrated widening of the tibiofibular clear space when the foot was in external rotation and dorsiflexion, with a narrowing of the tibiofibular clear space when the foot was in internal rotation and plantar flexion. The maximum clear space measurement recorded in an injured ankle, with the foot in external rotation, was 11 mm, with a maximum of 8.8 mm recorded in non-injured ankles. The findings of our study are, therefore, consistent with that of Barchilon et al.,12 who reported that a syndesmotic injury can be diagnosed confidently if there is a widening of the tibiofibular clear space, especially with forced eversion. Because the interosseous ligament plays a significant role in the stabilisation of the subtalar joint, dissection of this ligament results in a significant range of motion at the level of the subtalar joint. Anderson et al.19 similarly argued that 'a syndesmosis which widens under dynamic stress can be defined as unstable', based on the normal range of ankle joint motion that was demonstrated on cadavers before and after sectioning of the ligamentous structures. It can, thus, be concluded that rupture or dissection of the ligamentous structures of the ankle leads to instability in anterior translation along with rotational instability.19 Although injury to the syndesmosis is confirmed with clear space widening, care should be taken not to base the diagnosis solely on this feature without taking the imaging classifications of a normal ATiFL into consideration. Barchilon et al.12 further warn that in the absence of an ankle fracture, the clear space can easily be interpreted as normal. Only a few imaging modalities are consequently suitable to confirm the suspicion of a syndesmosis injury.
While this study provides useful information regarding the width of the tibiofibular clear space in our local population and, by implication, syndesmotic laxity, the main limitation of the study is the failure to grade the severity of the injury by only classifying findings as normal or abnormal.
Conclusion
Although MRI is still considered to be the best imaging modality for the diagnosis of soft tissue and intra-articular ankle pathology, our study confirms that technological advances in ultrasound have considerably increased its diagnostic value and enable qualified health care professionals to detect acute soft tissue pathology with equal clarity as MRI. Ultrasound could, therefore, be considered as one of the primary imaging modalities in the evaluation of the lateral ankle ligament complex and syndesmosis.
Acknowledgements
The authors wish to acknowledge Mr Lebo Tawane, Statkon, University of Johannesburg, for his statistical support.
Competing interests
The authors declare that they have no financial or personal relationship(s) that may have inappropriately influenced them in writing this article.
Authors' contributions
Mrs. van Niekerk was the primary investigator of this project. Mrs. van Dyk supervised the project and assisted with concept development, the research design, data analysis and interpretation.
References
1. Oae K, Ochi M, Takao M, Uchio Y. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. J Skeletal Radiol. 2010;39:41-47. https://doi.org/10.1007/s00256-009-0767-x [ Links ]
2. Lento PH, Primack S. Advances and utility of diagnostic ultrasound in musculoskeletal medicine. Curr Musculoskel Med. 2008;1:24-31. https://doi.org/10.1007/s12178-007-9002-3 [ Links ]
3. Van den Bekerom MPJ, Oostra RJ, Alvarez PG, Van Dijk CN. The anatomy in relation to injury of the lateral collateral ligaments of the ankle: A current concepts review. Clinical. Anatomy. 2008. 21:619-626. [ Links ]
4. Braman JE, Haut RC, Meyer EG, Post JM, Powell JW, Wei F. Eversion during external rotation of the human cadaver foot produces high ankle sprains. J Orthop Res. 2012;517:1-7. [ Links ]
5. Cha SD, Kim SS, Kwag HJ, Lee SY, Park HJ, Park NH, Rho MH. Accuracy of MRI findings in chronic lateral ankle ligament injury: Comparison with surgical findings. J Clin Radiol. 2012;67:313-318. https://doi.org/10.1016/j.crad.2011.08.025 [ Links ]
6. McLaurin T, Park JC. Acute syndesmosis injuries associated with ankle fractures. J NYU Hosp Joint Dis. 2009;67:39-43. [ Links ]
7. Beumer A, Swierstra A, Wagener ML. Chronic instability of the anterior tibiofibular syndesmosis of the ankle. Arthroscopic findings and results of anatomical reconstruction. J Musculoskel Dis. 2011;12:212-218. https://doi.org/10.1186/1471-2474-12-212 [ Links ]
8. Lin C-F, Gross MT, Weinhold P. Ankle syndesmosis injuries: Anatomy, biomechanics, mechanism of injury, and clinical guidelines for diagnosis and intervention. J Orthop Sports Phys Ther. 2006;36(6):372-384. https://doi.org/10.2519/jospt.2006.2195 [ Links ]
9. Harper MC, Keller TS. A radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle. 1989;10(3):156-160. https://doi.org/10.1177/107110078901000308 [ Links ]
10. Kennedy JG, Soffe KE, Dalla Vedova P, et al. Evaluation of the syndesmotic screw in low Weber C ankle fractures. J Orthop Trauma. 2000;14:359-366. https://doi.org/10.1097/00005131-200006000-00010 [ Links ]
11. Mulligan EP. Evaluation and management of ankle syndesmosis injury. Phys Ther Sports. 2011;12(2):57-69. https://doi.org/10.1016/j.ptsp.2011.03.001 [ Links ]
12. Barchilon V, Kots E, Mann G, Massarwe S, Mei-Dan O, Nysaka M. A dynamic ultrasound examination for the diagnosis of ankle syndesmotic injury in professional athletes. Am J Sports Med. 2009;37(5):1009-1016. https://doi.org/10.1177/0363546508331202 [ Links ]
13. Berlet C, Cottom JM, Hyer CFJ, Philbin TM. Transosseous fixation of the distal tibiofibular syndesmosis: Comparison of an introsseous suture and end button to traditional screw fixation in 50 cases. J Foot Ankle Surg. 2009;48(6):620-630. https://doi.org/10.1053/j.jfas.2009.07.013 [ Links ]
14. Ansede G, Healy JC, Lee JC. Musculoskeletal sonography of the normal foot. J Skeletal Radiol. 2010;39:225-242. https://doi.org/10.1007/s00256-009-0697-7 [ Links ]
15. Jacobson JA. Musculoskeletal ultrasound: Focused impact on MRI. Am J Radiol. 2009;193(3):619-627. https://doi.org/10.2214/AJR.09.2841 [ Links ]
16. De Maeseneer M, Jacobson JA, Jager T, et al. Sonography of the normal ankle: A target approach using skeletal reference points. Am J Roentgenol. 2009;192(2):487-495. https://doi.org/10.2214/AJR.08.1316 [ Links ]
17. Mei-Dan O, Carmont M, Laver L, et al. Standardization of the functional syndesmosis widening by dynamic U.S examination. BMC Sports Sci Med Rehabil. 2013;5:9. https://doi.org/10.1186/2052-1847-5-9 [ Links ]
18. Quatman CE, Ford KR, Myer GD. The effects of gender and maturational status on generalized joint laxity in young athletes. J Med Sci Sport. 2008;11:257. https://doi.org/10.1016/j.jsams.2007.05.005 [ Links ]
19. Anderson D, Bawab S, Dhakal A, Paranjape R, Ringleb SI. Effects of lateral ligament sectioning on the stability of the ankle and the subtalar joint. J Orthop Res. 2011;757:1459-1464. [ Links ]
 Correspondence:
Correspondence:
Barbara van Dyk
bvandyk@uj.ac.za
Received: 28 Feb. 2017
Accepted: 30 July 2017
Published: 29 Sept. 2017













